This is the second most popular article on this blog!
Look at the hits counter on this article...
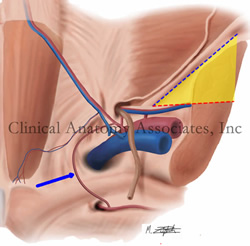
Image property of: CAA.Inc.. Artist: M. Zuptich.
The so-called "triangle of pain" is a misnomer coined by laparoscopic hernia surgeons who observed the anatomy of the inguinofemoral region from the posterior aspect and refers to an inverted "V" shaped area which should be avoided because of the potential to damage nerves when placing staples, tacks, or sutures to anchor a mesh during a laparoscopic herniorrhaphy.
An example of a similar situation with terminology is the so-called "triangle of doom". It is also not a triangle, as it only has two boundaries. similarly, it does indicate an area where it is dangerous to place staples or sutures during laparoscopic hernia surgery.
The "triangle of pain" is an inverted "V" shaped area with its apex at the internal (deep) inguinal ring. It is bound anteriorly by the iliopubic tract / inguinal ligament and by the testicular (spermatic) vessels posteromedially. This "triangle" has no defined posterolateral boundary. although you can see it in drawings by some authors.
The reason why this area should be avoided and not place staples or sutures to anchor a hernia mesh is that there are several nerves which usually cannot be seen as they run just deep to the endoabdominopelvic fascia.These nerves can suffer damage or entrapment when performing a laparoscopic herniorrhaphy and cause pain (hence the name of the area) as well as motor and sensory disorders.
The nerves are:
• Lateral femoral cutaneous nerve: arising from the ventral rami of L2 and L3, this nerve provides sensory innervation to the anterior skin of the thigh
• Femoral nerve: arising from the ventral rami of L2, L3, and L4, this nerves provides motor and sensory innervation to the anterior compartment of the thigh as well as sensory branches to the hip joint
• Genitofemoral nerve: arising from the ventral rami of L1 and L2, this nerve divides anterior to the psoas major muscle into two branches. The genital branch of the genitofemoral nerve enters the inguinal canal and provides sensory and motor innervation to the scrotum and cremaster muscle, as well as the labia majora and mons pubis. The femoral branch of the genitofemoral nerve enters the "triangle of pain" region and passes inferior to the inguinal ligament to provide sensory cutaneous innervation to the superior aspect of the thigh.
The image shows a posterior view of the inguinal region. The "triangle of pain" is depicted in yellow. The iliopubic tract / inguinal ligament is shown by a blue dotted line while the testicular vessels boundary is shown by a red dotted line. The blue arrow points to the aberrant obturator artery (Corona Mortis).
Thanks to Steve Pearson for suggesting this term. Medical illustration by Mark J. Zuptich.
Clinical anatomy of the inguinofemoral hernias, as well as abdominal and perineal hernias are some of the lecture topics developed and delivered to the medical devices industry by Clinical Anatomy Associates, Inc. For more information Contact Us.



