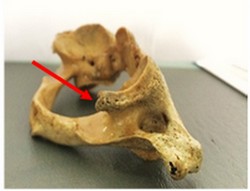
Figure A: Incomplete PP viewed from the
posterior aspect of the articular fossa
related to the retroglenoid tubercle
The Ponticulus Posticus (PP), also known as the pons arcuatus, foramen arcuale, and arcuate foramen, is a bony bridge that connects the retroglenoid tubercle with the posterior arch of the C1 vertebra, also known as the Atlas.
It substitutes the lateral segment of the posterior atlantooccipital ligament or joint capsule (1) on the area which stabilizes the vertebral artery on its emergency of the transverse foramen of the Atlas (2). This bridge or arch could be thick, thin or even incomplete (2). The importance of this calcification relies on the fact that it has been linked with cervicogenic headache (1,3) chronic tension-type headaches, sensorineural hearing loss (4), shoulder and arm pain, neck pain, and vertigo (1, 5).
The presence of a ponticulus posticus could also impact the planning of high cervical surgeries associated with the Atlas [C1] (6). A recent meta-analysis of the prevalence of this condition worldwide found an overall prevalence of a complete PP of 9.1% versus an incomplete PP, which was 13.6%. In males (10.4%) the complete PP was more common than in females (7.3%), but an incomplete PP was more commonly seen in females (18.5%) than in males (16.7%) (7).

Figure B: Complete PP. It crosses from the
retroglenoid tubercle down to the
posterior arch.
Despite the fact that this calcification has been associated with different painful disorders, some other authors consider it an anatomical condition destined to protect the vertebral artery and not a pathological condition (8). PP is visible on lateral cervical spine and cranial lateral radiographs as thin bony arch on the shape of a ring crossing from the retroglenoid tubercle to the posterior arch of C1, being either partially of fully calcified (Figures C and D).
Note 1: For the etymology of the term glenoid, click here.
Note 2: Figures C and D can be found at the bottom of the article
Sources:
1. Ross JS, Moore KR, editors. Diagnostic Imaging: Spine E-Book. 3rd ed. Philadeplphia: Elsevier; 2015. 31 p.
2. Torres Cueco R. La Columna Cervical: Evaluación Clínica y Aproximaciones Terapéuticas. Principios anatómicos, funcionales, exploración clínica y técnicas de tratamiento. Tomo I. 1° Ed. Madrid: Medica Panamericana; 2008. 124 p.
3. Tambawala SS, Karjodkar FR, Sansare K, Motghare D, Mishra I, Gaikwad S, Dora AC. Prevalence of Ponticulus Posticus on Lateral Cephalometric Radiographs, its Association with Cervicogenic Headache and a Review of Literature. World Neurosurg [Internet]. 2017 Apr 17(cited 02 Jun 2017). pii: S1878-8750(17)30525-9. Available at: doi: 10.1016/j.wneu.2017.04.030. [Epub ahead of print]
4. Koutsouraki E, Avdelidi E, Michmizos D, Kapsali SE, Costa V, Baloyannis S. Kimmerle's anomaly as a possible causative factor of chronic tension-type headaches and neurosensory hearing loss: Case report and literature review. Int J Neurosci. 2010; 120:236-9
5. Cakmak O, Gurdal E, Ekinci G, Yildiz E, Cavdar S. Arcuate foramen and its clinical significance. Saudi Med J. 2005; 26:1409-13.
6. Song MS, Lee HJ, Kim JT, Kim JH, Hong JT. Ponticulus posticus: Morphometric analysis and Its anatomical Implications for occipito-cervical fusion. Clin Neurol Neurosurg [Internet]. 2017 Jun (cited 02 Jun 2017);157:76-81. Available at: doi: 10.1016/j.clineuro.2017.04.001. Epub 2017 Apr 3.
7. Pękala PA, Henry BM, Pękala JR, Hsieh WC, Vikse J, Sanna B, Walocha JA, Tubbs RS, Tomaszewski KA. Prevalence of foramen arcuale and its clinical significance: a meta-analysis of 55,985 subjects. J Neurosurg Spine [Internet]. 2017 Jun (cited 02 Jun 2017); 16:1-15. Available at: doi: 10.3171/2017.1.SPINE161092. [Epub ahead of print]
8. Schilling J, Schilling A, Suazo I. Ponticulus posticus on the Posterior Arch of Atlas, Prevalence Analysis in Asymptomatic PatientsInt. J. Morphol. 2010 Mar; 28(1):317-322.
Acknowledgments: The Atlas [C1] specimens shown on figures A and B belong to the Anatomy department of the Medical College of the Finis Terrae University, Santiago, Chile and are used to show two examples of PP. With permission.
Article written by Prof. M. Fernanda Cortes, DDS, MsC.
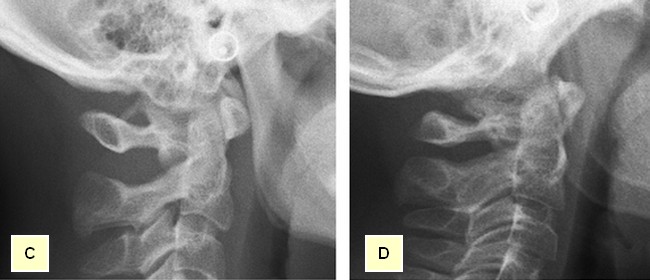 Figure C: Complete PP shown on a lateral radiographic view. Figure D: Partial PP shown on a lateral radiographic view.
Figure C: Complete PP shown on a lateral radiographic view. Figure D: Partial PP shown on a lateral radiographic view.



