Medical Terminology Daily (MTD) is a blog sponsored by Clinical Anatomy Associates, Inc. as a service to the medical community. We post anatomical, medical or surgical terms, their meaning and usage, as well as biographical notes on anatomists, surgeons, and researchers through the ages. Be warned that some of the images used depict human anatomical specimens.
You are welcome to submit questions and suggestions using our "Contact Us" form. The information on this blog follows the terms on our "Privacy and Security Statement" and cannot be construed as medical guidance or instructions for treatment.
We have 204 guests and no members online

Jean George Bachmann
(1877 – 1959)
French physician–physiologist whose experimental work in the early twentieth century provided the first clear functional description of a preferential interatrial conduction pathway. This structure, eponymically named “Bachmann’s bundle”, plays a central role in normal atrial activation and in the pathophysiology of interatrial block and atrial arrhythmias.
As a young man, Bachmann served as a merchant sailor, crossing the Atlantic multiple times. He emigrated to the United States in 1902 and earned his medical degree at the top of his class from Jefferson Medical College in Philadelphia in 1907. He stayed at this Medical College as a demonstrator and physiologist. In 1910, he joined Emory University in Atlanta. Between 1917 -1918 he served as a medical officer in the US Army. He retired from Emory in 1947 and continued his private medical practice until his death in 1959.
On the personal side, Bachmann was a man of many talents: a polyglot, he was fluent in German, French, Spanish and English. He was a chef in his own right and occasionally worked as a chef in international hotels. In fact, he paid his tuition at Jefferson Medical College, working both as a chef and as a language tutor.
The intrinsic cardiac conduction system was a major focus of cardiovascular research in the late nineteenth and early twentieth centuries. The atrioventricular (AV) node was discovered and described by Sunao Tawara and Karl Albert Aschoff in 1906, and the sinoatrial node by Arthur Keith and Martin Flack in 1907.
While the connections that distribute the electrical impulse from the AV node to the ventricles were known through the works of Wilhelm His Jr, in 1893 and Jan Evangelista Purkinje in 1839, the mechanism by which electrical impulses spread between the atria remained uncertain.
In 1916 Bachmann published a paper titled “The Inter-Auricular Time Interval” in the American Journal of Physiology. Bachmann measured activation times between the right and left atria and demonstrated that interruption of a distinct anterior interatrial muscular band resulted in delayed left atrial activation. He concluded that this band constituted the principal route for rapid interatrial conduction.
Subsequent anatomical and electrophysiological studies confirmed the importance of the structure described by Bachmann, which came to bear his name. Bachmann’s bundle is now recognized as a key determinant of atrial activation patterns, and its dysfunction is associated with interatrial block, atrial fibrillation, and abnormal P-wave morphology. His work remains foundational in both basic cardiac anatomy and clinical electrophysiology.
Sources and references
1. Bachmann G. “The inter-auricular time interval”. Am J Physiol. 1916;41:309–320.
2. Hurst JW. “Profiles in Cardiology: Jean George Bachmann (1877–1959)”. Clin Cardiol. 1987;10:185–187.
3. Lemery R, Guiraudon G, Veinot JP. “Anatomic description of Bachmann’s bundle and its relation to the atrial septum”. Am J Cardiol. 2003;91:148–152.
4. "Remembering the canonical discoverers of the core components of the mammalian cardiac conduction system: Keith and Flack, Aschoff and Tawara, His, and Purkinje" Icilio Cavero and Henry Holzgrefe Advances in Physiology Education 2022 46:4, 549-579.
5. Knol WG, de Vos CB, Crijns HJGM, et al. “The Bachmann bundle and interatrial conduction” Heart Rhythm. 2019;16:127–133.
6. “Iatrogenic biatrial flutter. The role of the Bachmann’s bundle” Constán E.; García F., Linde, A.. Complejo Hospitalario de Jaén, Jaén. Spain
7. Keith A, Flack M. The form and nature of the muscular connections between the primary divisions of the vertebrate heart. J Anat Physiol 41: 172–189, 1907.
"Clinical Anatomy Associates, Inc., and the contributors of "Medical Terminology Daily" wish to thank all individuals who donate their bodies and tissues for the advancement of education and research”.
Click here for more information
- Details
- Written by: Efrain A. Miranda, Ph.D.
This article is part of the series "A Moment in History" where we honor those who have contributed to the growth of medical knowledge in the areas of anatomy, medicine, surgery, and medical research.
Further to my comment on old books and research that started with an interesting bookplate (Ex-Libris). I continued my research and found that the person in charge of the Osler library bookplate was a fascinating individual that today maybe a ghost in the MedChi library and building in Baltimore... This is certainly an article that can be called "A Moment in History"
Marcia Crocker Noyes was the librarian at The Maryland State Medical Society from 1896 to 1946 and was a founding member of the Medical Library Association.[1][2][3]
Sir William Osler, MD. a famous Johns Hopkins surgeon was a noted bibliophile and had a large personal collection of books on various topics. When he became the President of MedChi in 1896, he was dismayed at the condition of the library and knew that with the right person and some stewardship, it could become a significant collection. Sir William asked his friend, Dr. Bernard Steiner, a physician and President of the Enoch Pratt Free Library in Baltimore for suggestions of a librarian, and Dr. Steiner recommended Marcia Crocker Noyes. A native of New York, and a graduate of Hunter College, Marcia had moved to Baltimore for a lengthy visit with her sister, and took a “temporary” position at the Pratt Library, which turned into three years. Although she had no medical experience or background, she was enthusiastic, and most importantly, she was willing to move into the apartment provided for the librarian, who needed to be available 24 hours a day.
The image in this article is Ms. Noyes on her first year on the job. Marcia developed a book classification system for medical books, based on the Index Medicus, and called it the Classification for Medical Literature. The system uses the alphabet with capital letters for the major divisions of medicine and lower-case ones for the sub-sections. The system was used for many years, but it's now dated and the Faculty's original shelving scheme was never changed. The card catalogs still reflect her classification and many of the cards are written in Marcia's back-slanting handwriting.
Marcia knew enough to ask the Faculty's members about medical questions, terminology and literature. She gradually won over the predominantly male membership and they became her greatest allies; Sir William at the start, and then for nearly 40 years, Dr. John Ruhräh, a wealthy pediatrician with no immediate family of his own. She made a point of attending almost every Faculty function, and in 1904, under guidelines from the American Medical Association, Marcia was made the Faculty Secretary. For much of her first 10 years, she was the Faculty's only full-time employee, only being assisted by Mr. Caution, the Faculty's janitor. Later in life Marcia would say that she hired him because of his name!
Within ten years, the library had outgrown its space, and plans, spearheaded by Marcia and Sir William before his move to Oxford, were made to build a headquarters building, mainly to house the library's growing collection of medical books and journals.
Marcia was instrumental in the design and building of the new headquarters. She travelled to Philadelphia, New York and Boston to look at their medical society buildings, and eventually, the Philadelphia architectural firm, Ellicott & Emmart was selected to design and build the new Faculty building. Every detail of the building held her imprimatur, from the graceful staircase, to the light-filled reading room, and all of the myriad details of the millwork, marble tesserae, and most of all, the four-story cast iron stacks. She was on-site, climbing up unfinished staircases, checking out the progress of the building, which was built in less than one year at a cost of $90,000.
Among the features of the new building was a fourth-floor apartment for her. She referred to it as the "first penthouse in Baltimore" and it had a garden and rooftop terrace. The library collection eventually grew to more than 65,000 volumes from medical and specialty societies around the world. Journals were traded back and forth, and physicians eagerly anticipated the arrival of each new issue. At the same time, Marcia was involved in the Medical Library Association as one of eight founding members. The MLA promotes medical libraries and the exchange of information. One of the earliest mandates of the MLA was the Exchange, a distribution and trade service for those who had duplicates or little-used books in their collections. Initially, the Exchange was run out of the Philadelphia medical society, but in 1900 it was moved to Baltimore and Marcia oversaw it. Several hundred periodicals and journals were received and sent each month, a huge amount of work for a tiny staff. In 1904, the Faculty had run out of room to manage the Exchange, so it was moved to the Medical Society of the Kings County (Brooklyn). But without Marcia's excellent administrative skills, it floundered and in 1908, the MLA asked Marcia to take charge once again.
 In 1909, when the new Faculty building opened, there was enough room to run the Exchange and with the help of MLA Treasurer, noted bibliophile and close friend, Dr. John Ruhräh, it once again became successful. Additionally, Marcia and Dr. Ruhräh combined forces to revive the MLA's bulletin, which had all but ceased publication in 1908, taking the Exchange with it. This duo maintained editorial control from 1911 until 1926. In 1934, around the time of Dr. Ruhräh's death, Marcia became the first “unmedicated” professional to head the MLA. During her tenure, the MLA incorporated, the first seal was adopted, and the annual meeting was held in Baltimore. Marcia wanted to write the history of the MLA once she retired from full-time work at the Faculty, but her health was beginning to fail. She had back problems and had suffered a serious burn on her shoulder as a young woman, possibly from her time running a summer camp, Camp Seyon, for young ladies in the Adirondack Mountains. In 1946, a celebration was planned to honor Marcia's 50 years at the Faculty. But she was adamant that the physicians wait until November, the actual date of her 50 years. However, they knew she was gravely ill, and might not make it until then, so a huge party was held in April. More than 250 physicians attended the celebration, but the ones she was closest to in the early years, were long gone. She was presented with a suitcase, a sum of money to use for travelling, and her favorite painting of Dr. John Philip Smith, a founder of the Medical College in Winchester, Virginia. It was painted by Edward Caledon Smith, a Virginia painter who had been a student of the painter Thomas Sully.[4] She adored this painting and vowed, jokingly, to take it with her wherever she went.
In 1909, when the new Faculty building opened, there was enough room to run the Exchange and with the help of MLA Treasurer, noted bibliophile and close friend, Dr. John Ruhräh, it once again became successful. Additionally, Marcia and Dr. Ruhräh combined forces to revive the MLA's bulletin, which had all but ceased publication in 1908, taking the Exchange with it. This duo maintained editorial control from 1911 until 1926. In 1934, around the time of Dr. Ruhräh's death, Marcia became the first “unmedicated” professional to head the MLA. During her tenure, the MLA incorporated, the first seal was adopted, and the annual meeting was held in Baltimore. Marcia wanted to write the history of the MLA once she retired from full-time work at the Faculty, but her health was beginning to fail. She had back problems and had suffered a serious burn on her shoulder as a young woman, possibly from her time running a summer camp, Camp Seyon, for young ladies in the Adirondack Mountains. In 1946, a celebration was planned to honor Marcia's 50 years at the Faculty. But she was adamant that the physicians wait until November, the actual date of her 50 years. However, they knew she was gravely ill, and might not make it until then, so a huge party was held in April. More than 250 physicians attended the celebration, but the ones she was closest to in the early years, were long gone. She was presented with a suitcase, a sum of money to use for travelling, and her favorite painting of Dr. John Philip Smith, a founder of the Medical College in Winchester, Virginia. It was painted by Edward Caledon Smith, a Virginia painter who had been a student of the painter Thomas Sully.[4] She adored this painting and vowed, jokingly, to take it with her wherever she went.
The painting was not to stay with her for very long, for she died in November 1946, and left it to the Faculty in her will. Her funeral was held in the Faculty's Osler Hall, named for her dear friend. More than 60 physicians served as her pallbearers, and she was buried at Baltimore's Green Mount Cemetery. In 1948, the MLA decided to establish an award in the name of Marcia Crocker Noyes. It was for outstanding achievement in medical library field and was to be awarded every two years, or when a truly worthy candidate was submitted. In 2014, the Faculty began giving a bouquet of flowers to the winner of the award in Marcia's name, and in honor of her work. Much evidence exists for this tradition, as we know that the physicians, especially Drs. Osler and Ruhräh, frequently gave her bouquets of flowers. Marcia also cultivated flower gardens at the Faculty and decorated the rooms with her work.
Today, the MedChi building is open for tours and if the rumors are to be believed Ms. Marcia Crocker Noyes is still at work in her beloved library as the "resident ghost" [1][5]
NOTE: This article has been modified from the original Wikipedia article on Marcia Crocker Noyes. The article itself is well-written with interesting images of the subject. I would encourage you to visit it. The second insert is from book ML-0736 in my personal library and shows in pencil, the incredibly small handwriting of Marsha C. Noyes.
Sources:
1. "Marcia, Marcia, Marcia" MedChi Archives blog.
2. "Marcia C. Noyes, Medical Librarian" (PDF). Bulletin of the Medical Library Association. 35 (1): 108–109. 1947. PMC 194645
3. Smith, Bernie Todd (1974). "Marcia Crocker Noyes, Medical Librarian: The Shaping of a Career" (PDF). Bulletin of the Medical Library Association. 62 (3): 314–324. PMC 198800Freely accessible. PMID 4619344.
4. Edward Caledon BRUCE (1825-1901)"
5. Behind the scenes tour MedChiBuilding
- Details
- Written by: Prof. C. Uribe
The following article was written by contributor anatomists from Chile. Many of the words and concepts used are specific to Spanish, so we decided to publish the article in its original language. For any comments, please contact the authors.
Key Words: Anatomical Terminology, Nomenclature Anatomical, Eponym
Fundamentos para la utilización de la terminología anatómica
1. Abstract / Resumen
2. Introducción
3. Terminología y Nomenclatura
4. Antecedentes Históricos
5. Nomenclaturas Anatómicas
6. Términos
7. Consideraciones Finales
8. Conclusiones
9. Bibliografía
Abstract
This revision points to clear the evident problem between anatomy professors, professionals and clinical professors, this is, the existence of inaccurate, complex or unspecific anatomical terms, besides the existence and persistence of eponyms and synonyms, a problem which harms pre-grad students in its initial formative process This Semantic definitions will be given, and the acquisition of new anatomic nomenclatures and terminologies will be situated within an historical context, looking with this, justification to the actual “Anatomical terminology”, which has for objective to displace the old “Nomina Anatomica”. In the final section, anatomical terms examples will be given, contrasting the old term with the one actual anatomical terminology suggests. (Back to top)
Resumen
Esta revisión apunta a dar luz sobre un problema evidente entre docentes de Anatomía Humana, profesionales y docentes clínicos, la existencia de términos anatómicos inexactos, complejos o inespecíficos, además de la existencia de Epónimos y Sinonimia, problema del cual los más perjudicados son los alumnos de pregrado en sus procesos formativos iniciales. Se darán definiciones semánticas y se situará dentro de un contexto histórico la adquisición de nuevas nomenclaturas y terminologías Anatómicas, buscando con esto justificación a la actual “Terminología Anatómica” la cual tiene por objetivo el desplazar la antigua “Nomina Anatómica”.
En la parte final se entregarán ejemplos característicos de términos anatómicos, enfrentando el término antiguo con el que sugiere la actual terminología anatómica. (Back to top)
Palabras Claves: Terminología Anatómica, Nomenclatura Anatómica, Epónimos
Introducción
La anatomía es la ciencia que se preocupa de estudiar la forma, conformación y las interrelaciones de todas las estructuras corporales. Al estudiarla sentamos las bases para la compresión de un individuo bajo un concepto de normalidad. De aquí la gran importancia de la disciplina, ya que posteriormente con esta importante base de conocimiento se puede comprender y tratar la anormalidad.
Un fenómeno frecuente que subyace a todo tipo de lenguaje es la existencia de varios términos para designar un mismo concepto (sinonimia) y además de la posibilidad de que un mismo término pueda poseer varios significados (polisemia) (1). En el lenguaje científico y médico esto es común, con mayor razón en las ciencias morfológicas y de ellas, la anatomía es particularmente la que en términos prácticos genera la mayor cantidad de controversias y desencuentros, ya que los términos usados en clínica, en referencia a estructuras corporales tienen su origen en la terminología anatómica y son de uso diario.
A la gran cantidad de términos anatómicos existentes se suma las confusiones generadas cuando en algunos países y en otras ocasiones, traductores de escritos anatómicos, le asignan un nombre diferente a cada estructura o elemento. Esto lleva a escuchar habituales quejas de profesionales y alumnos frente a “un término” expresado de diferentes formas, ya sea, por los diferentes profesores de anatomía o por los docentes y ayudantes en el pabellón y laboratorio anatómico. Particularmente, en nuestro medio, esta situación es una constante, ya que debemos responder a dialécticas regionales e internacionales, producto de la literatura que recibimos desde el extranjero.
Con los años esto ha generado un conflicto en el desarrollo científico y divulgación de las ciencias morfológicas, separando progresivamente a los docentes de anatomía con los profesionales clínicos. (14)
En el transcurso de esta revisión se darán definiciones semánticas y se situará dentro del contexto histórico la adquisición de diversas nomenclaturas y terminologías, hasta llegar al último gran esfuerzo por consensuar los términos anatómicos, la “Terminología Anatómica” la cual en la actualidad ha desplazado a la anteriormente llamada “Nómina Anatómica”.
En la última parte se hará referencia a términos de uso habitual, fundamentalmente del aparato musculoesquelético, de mayor uso en el quehacer kinésico, enfrentando el termino antiguo con el que sugiere la actualizada terminología anatómica.
(Back to top)
Terminología y Nomenclatura
La palabra terminología puede entenderse de diferentes maneras: en primer lugar, la terminología es el conjunto de vocabulario especial de una disciplina o un ámbito de conocimiento; en segundo lugar, la terminología puede entenderse como una disciplina, que tiene por objeto la construcción de una teoría de los términos, el estudio de los mismos, su recopilación y sistematización en glosarios especializados como las nomenclaturas. (2-5) (12) (16).
El problema terminológico no es nuevo para anatomía, han transcurrido más de 100 años desde que se inició un proceso que busca la unificación de criterios a nivel internacional (6), que consiste en priorizar un término sobre el resto de los equivalentes, mediante la elección de un término único, como el aceptable para designar un solo concepto, rechazando con esto los anteriores sinónimos. (7)
Con este objetivo surgen las nomenclaturas que son un tipo de terminología aplicada a cosas naturales u objetos que forman series más o menos homogéneas cuyas denominaciones se crean conforme a reglas uniformes. Se crean con el objetivo de reducir al máximo la diversidad terminológica, escogiendo el término que posea mayor fuerza descriptiva, mayor simplicidad y especificidad. (1, 2, 5)
La construcción de estas nomenclaturas médicas, así como de listas de términos y glosarios normativos (aprobados por autoridades científicas oficiales), que aspiran a lograr la uniformidad terminológica en la denominación de conceptos, parten de la idea que la variación es un perjuicio para la comunicación y de que es imprescindible establecer una terminología única y aceptable para todos los sectores implicados en la comunicación médica, como docentes, investigadores, redactores, traductores, correctores, editores, bibliotecarios y otros. (1, 2,8,9)
Autores, como A. Manuila y diversos expertos de la OMS, consideran que la diversidad deja sumida a la terminología en un estado de “confusión” tal, que se convierte en un obstáculo para el propio “progreso” de la ciencia. Hacen referencia estos autores que un término como mielofibrosis tiene 12 sinónimos en inglés, y el correspondiente en alemán posee 13, y en francés existen 31 términos equivalentes del mismo. Esta situación es calificada por dicho especialista como de “desorden”, en la medida en que es un obstáculo para la comparabilidad de los datos y el almacenamiento y recuperación de la información médica. (9,10).
(Back to top)
Antecedentes Históricos
La evolución sufrida por el lenguaje anatómico es el fiel reflejo de la experiencia histórica de los pueblos y de su desarrollo cultural. Sus cambios semánticos y ortográficos, metáforas, mezclas lingüísticas, conflictos nacionalistas y personalistas por la primacía en las denominaciones, impropiedades léxicas, paronimias y sinonimias, expresan esta rica diversidad. (8).
Es casi imposible sustraerse de estos puntos. Felipe Mellizo expresa en “Literatura y enfermedad”: El profesor de anatomía nombraba en latín las partes, intrigantes, magníficas, del cuerpo, y eso permitía, eso permite, que todos comprendamos que allí no es sólo anatomía lo que se explica, sino que se está explicando también la historia de la cultura. (8,11)
Como es sabido, durante la Antigüedad y la Baja Edad Media, la lengua de la Anatomía, como de toda la ciencia, era el griego, y en menor medida el latín. A partir del siglo XI, la presencia de los árabes en Europa llevó a la realización de traducciones y adaptaciones al latín de textos árabes que contenían el lenguaje clásico (latín). El desconocimiento de terminología latina obligo a introducir por parte de los traductores, términos árabes. Con la llegada del Renacimiento se llevo a cabo una restitución de los textos griegos y latinos originales, recuperando la terminología (6).
Los descubrimientos anatómicos posteriores, con bases más sujetas a la experimentación y la observación directa, traen como consecuencia la aparición de neologismos, no siempre bien construidos, además de numerosos epónimos (dar nombre a una estructura con el apellido o nombre del descubridor) con las consiguientes pugnas en la autoría de los hallazgos anatómicos. (8)
En este aspecto es sorprendente la riqueza metafórica del léxico anatómico y con una semánticas apegada a la realidad humana y a la vida cotidiana: acetabulum designaba un recipiente para contener vinagre; alveolus viene del latín alveus ‘colmena’; amígdala procede del griego Amygdala ‘almendra’; clítoris era para los griegos una colina o pequeño promontorio; gínglimo procede del griego ginglymós ‘gozne’. Inclusive hay metáforas vegetales, animales, geográficas o domésticas que revelan esta tendencia tan humana expresada en el léxico anatómico, estructuras como “deltoides”, “bipenado”, unipenado” dentro de muchas más. (8).
(Back to top)
Nomenclaturas Anatómicas
Los primeros análisis con respecto a la terminología se inician en 1887 en Leipzig, Alemania, continuándose en el Reino Unido en 1894. Producto de esto y después de siglos de acumulación de términos anatómicos se junta un grupo de anatomistas alemanes (el líder fue Wilhelm His) en Basilea en 1895 dando fruto a la primera Nomenclatura Anatómica Internacional con el nombre de Nomina Anatómica; en inglés suelen referirse a ella como Basle Nomina Anatomica o BNA (Nomenclatura Anatómica [Internacional] de Basilea)(6). Fundamentalmente trata de eliminar diferencias nacionales, en forma honorífica mantiene el nombre de uno o más científicos que hubiesen sido los primeros en describir una estructura. En la práctica, sólo se impuso entre los profesionales de habla alemana y en gran parte de Norteamérica. (6).
Con anterioridad a la II Guerra Mundial, se publicaron de forma casi simultánea una revisión británica (The Birmingham Revision, BR, en 1933) y otra alemana (Jenaer Nomina Anatomica, JNA, en 1935) que vinieron a complicar más aún la situación. De ellas, la que alcanzó más importancia fue la alemana y conocida en inglés como Jena Nomina Anatomica o JNA. (6)
En el V Congreso Federativo Internacional de Anatomía que fue llevado a cabo en Oxford, Inglaterra, en 1950 y en un intento de uniformar la nomenclatura anatómica, la Federación Internacional de Asociaciones de Anatomistas (FIAA) creó un Comité Internacional de Nomenclatura Anatómica que elaboró una nueva nomenclatura latina internacional, aprobada en 1955 con motivo del VI Congreso Federativo Internacional de Anatomía, que se celebró en París, aparece la Parisiensia Nomina Anatomica o, en inglés, Paris Nomina Anatómica o PNA (Nomenclatura Anatómica [Internacional] de París). De hecho cuando se hace referencia en los textos anatómicos de final del siglo XX a la expresión Nomina Anatómica a secas, casi siempre hace referencia a esta Nomenclatura Anatómica de París. En los congresos mundiales anatómicos de Nueva York (1960), Wiesbaden (1965), Tokio (1975) y México (1980) se efectuaron revisiones y nuevas ediciones a la nómina. Lamentablemente las referencias para estas revisiones son muy confusas ya que por ejemplo tras el congreso de Tokio, algunos autores de lengua inglesa hablaban de Nomina Anatomica 4th edition (o Paris Nomina Anatomica 4th edition), mientras que otros preferían hablar de Tokyo Nomina Anatomica. Y eso sin tener en cuenta las comunes confusiones con nuevas ediciones de reimpresiones en los diferentes países. Una disputa en 1985 entre la FIAA y el Comité Internacional de Nomenclatura Anatómica terminó con la ruptura de relaciones entre ambos organismos en 1989, cuando el Comité publicó la sexta edición de los Nomina Anatómica sin someterla a la aprobación del XIII Congreso Federativo Internacional de Anatomía celebrado en Río de Janeiro. En agosto de 1989, la FIAA decidió crear un nuevo Comité Federal de Terminología Anatómica con el encargo de elaborar una nueva nomenclatura anatómica internacional. En Lisboa 1994 se incorpora el idioma ingles como valido dentro de la terminología. Tras varias reuniones, el nuevo Comité publicó en 1998 la nueva Terminología Anatómica (Terminología Anatómica Internacional), que hoy ha sustituido a la Nomina Anatómica como nomenclatura anatómica oficial en todo el mundo. (6)
En la actualidad existe el Comité Internacional Mundial que revisa la Terminología en Histología y Embriología, además de la terminología Veterinaria.
(Back to top)
Términos
Con el interés de ejemplificar los cambios generados por la Terminología Anatómica, haremos referencia a términos de uso común en la jerga anatómica y clínica los cuales deberían según la terminología anatómica ser sustituidos:
Anatomía General
Partes del cuerpo
Extremidad superior cambiar por Miembro superior
Extremidad inferior cambiar por Miembro inferior
Cintura escapular cambiar por Cintura o Cíngulo Pectoral
Términos descriptivos
Borde externo cambiar por Borde o Margen lateral
Borde interno cambiar por Borde o Margen medial
Sistema esquelético
Apófisis cambiar por Proceso
Escotadura cambiar por Incisura
Maxilar superior cambiar por Maxila - Maxilar
Maxilar inferior cambiar por Mandíbula
Agujero cambiar por Agujero o Foramen
Omoplato cambiar por Escápula
Cubito cambiar por Úlna
Peroné cambiar por Fibula
Rotula cambiar por Patela
Astrágalo cambiar por Talo
Escafoides Tarsiano cambiar por Navicular
Articulación tipo Diartrosis cambiar por Art. Sinovial o Diartrosis
Articulación tipo Trocoide cambiar por Articulación Pivote
Articulación tipo Ginglimo cambiar por Articulación Bisagra
Articulación tipo Enartrosis cambiar por Art. Enartrosis o Esferoidea
Articulación tipo artrodias cambiar por Articulación plana
Músculos
Cubital Anterior cambiar por Flexor Ulnar del Carpo
1er Radial cambiar por Extensor Radial largo del Carpo
Supinador Largo cambiar por Braquiorradial
Extensor común de los dedos cambiar por Extensor de los dedos
Recto interno cambiar por Grácil
Epónimos
Órgano de Corti cambiar por Órgano espiral
Articulación de Chopart cambiar por Art. transversa del tarso
Ligamento de Bertin cambiar por Ligamento Iliofemoral
Fondo de Douglas cambiar por Excavación rectouterina o rectovesical
Nódulo de Aschoff-Tawara cambiar por Nodo atrioventricular
Nódulo de Keith-Flack cambiar por Nodo sinoatrial
Trompa de Falopio cambiar por Tuba uterina
Trompa de Eustaquio cambiar por Tuba auditiva
(Back to top)
Consideraciones Finales
Hay que estar consciente de que, en países como Francia y España, países de los cuales recibimos mucha bibliografía clínica la nomenclatura anatómica internacional no ha conseguido desplazar aún a la nomenclatura anatómica tradicional. Así, por ejemplo, el término internacional fibula para los españoles, sigue siendo ‘peroné’; El músculo Braquiorradial (musculus brachioradialis del latín) es ‘músculo supinador largo’; la arteria Carótida Común (arteria carotis communis) es ‘arteria carótida primitiva’; líquido cerebro espinal (liquor cerebrospinalis) es ‘líquido cefalorraquídeo’; Nervio fibular común (nervus fibularis communis) es ‘nervio ciático poplíteo externo’ y Linfonodos (nodus lymphaticus) es ‘ganglio linfático’. (8)
Es loable el esfuerzo que se hace a favor de una terminología universal, es el caso reciente de la cumbre de Terminología en el año 2002 en la que representantes de instituciones, organismos y redes de terminología de distinta índole, dieron fruto a la declaración de Bruselas, solicitando a los estados y organismos internacionales que en el marco de su política lingüística apoyen la creación de estructuras básicas de terminología, promuevan el desarrollo y la actualización de los recursos terminológicos, así como el acceso gratuito a las terminologías y en particular a aquella utilizada en los documentos oficiales de los gobiernos e instituciones internacionales. Si bien esto esta enfocado a políticas gubernamentales y de las tecnologías de la información se observa la tendencia actual a los consensos lingüísticos. En efecto, el conocimiento y empleo de las terminologías científicas tiene un impacto importante y creciente en el mundo globalizado, en el que las comunicaciones entre especialistas y usuarios procedentes de comunidades lingüísticas diversas se han vuelto una necesidad imperiosa. (13,15)
(Back to top)
Conclusiones
Así a 110 años de esfuerzo por unificar internacionalmente los términos usados en Anatomía exhortamos a alumnos, docentes y clínicos a usar la Terminología Anatómica, con lo que evitaríamos, ese estado de “confusión”, que se convierte en un obstáculo para el progreso de la ciencia.
El estudio de los procesos y antecedentes históricos nos aportan datos valiosos; una estructura habla de sí misma producto de su historia terminológica. Ortega y Gasset consideraban a las palabras como “algos humanos vivientes”, de ahí que afirmara que “cada palabra reclama una biografía”.
En una sociedad como la nuestra, que no siempre es capaz de reconocer que la investigación humanística exige el mismo rigor y profesionalidad que la investigación científica, hay que valorar los esfuerzos tendientes a consensuar las dos disciplinas y pensando siempre en el fortalecimiento de la Anatomía como ciencia fundamental y pilar del conocimiento de los profesionales de ciencias biomédicas.
(Back to top)
Bibliografía:
(1) Díaz Rojo, J. La terminología médica: diversidad, norma y uso. Panace. 2001; vol. 2 (4):40-48.
(2) Cabré, M. T. La terminología. Teoría, metodología y aplicaciones. Barcelona: Editorial Antárdia/Empúries; 1993.
(3) Cabré, M.T. Elementos para una teoría de la terminología: hacia un paradigma alternativo. El Lenguaraz Revista académica del Colegio de Traductores Públicos de la Ciudad de Buenos Aires. 1998; vol 1 (1):59-78
(4) Cabré, M.T. Hacia una teoría comunicativa de la terminología: Aspectos metodológicos. La terminología representación y comunicación. Barcelona: IULA; 1999.p. 129-150
(5) Cabré, M.T. La terminología, una disciplina en evolución: pasado y algunos elementos de futuro. Debate Terminológico. 2008. Disponible en: www.riterm.net/revista/n_1/cabre.pdf
(6) FEDERATIVE COMMITTEE ON ANATOMICAL TERMINOLOGY. (FCAT). Terminología anatómica. Stuttgart, Georg Thieme Verlag; 1998.
(7) Wüster E. Introducción a la teoría de la terminología y a la lexicografía terminológica. Barcelona: IULA; 1998.
(8) Díaz Rojo, J., Juan José Barcia Goyanes (1901-2003), estudioso de la historia del lenguaje anatómico. Panace. 2003; Vol.4 , Nº (13–14).
(9) Manuila A. Progress in Medical Terminology. Basilea: Karger; 1981.
(10) Stewart WH. Towards uniformity in medical nomenclature. Statement by Surgeon General of the United States to WHO in May 1966. En: Manuila A. Progress in Medical Terminology. Basilea: Karger, 1981.
(11) Mellizo F., Literatura y enfermedad. Barcelona: Plaza y Janés; 1979.
(12) Temmerman, R. Towards new ways of terminology description: the socio-cognitive approach. Amsterdam/Philadelphia: John Benjamins; 2000.
(13) Schnell B., Rodriguez N., La terminología: nuevas perspectivas y futuros horizontes. ACTA. 2008. Disponible en: www.acta.es
(14) Whitmore I. Terminologia Anatomica: new terminology for the new anatomist. Anat Rec (New Anat.) 1999; 257: 50-53.
(15) Rosse C, Terminologia Anatomica; Considered from the Perspective of Next-Generation Knowledge Sources. Clin Anat. 2001;14(2):120-33
(16) Weissenhofer, P. Conceptology in Terminology Theory, Semantics and Word Formation. Viena: TermNet.,1995.
(Back to top)
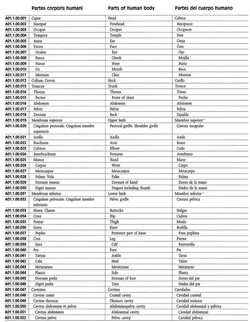
La imagen en este articulo es una página selecionada de la Terminologia Anatomica ilustrando la organización jerárquica que tiene el libro. Nótese la columna izquierda que indica el código de cada estructura.
Agradecimientos
Se agradece la exhaustiva revisión, comentarios y aportes del Profesor Dr. Alberto Rodríguez Torres, de la Facultad de Medicina de la Universidad de Chile.
Autores:
Cristián Uribe Vásquez
Kinesiólogo, Magíster en Ciencias Anatomía Humana
Docente, Universidad Andrés Bello – Chile
Rodolfo Sanzana Cuche
Kinesiólogo, Magíster Morfología Humana
Docente, Universidad de Chile
- Details
UPDATED: The root term [-zyg-] originates from the Greek [ζεύγος] meaning "a pair", as in a yoke. Applications of this root term include:
• Azygos: The prefix [a-] means "no", "not", or "without". Not paired or unyoked. The azygos system of veins, found in the posterior aspect of the mediastinum, is not symmetrical. It is therefore "unpaired". It is composed of dissimilar contralateral components which include the azygos vein on the right side, and the hemiazygos and accessory hemiazygos on the left side.
• Hemiazygos: The prefix [-hemi-] means "half". Half unpaired or unyoked. Refers to the contralateral component of the azygos system of veins.
• Zygapophysis: Click on the link for more information. Paired (bilateral) bony articular protrusions in the posterior aspect of the vertebrae
Important note to medical writers: The word is "azygos", not "azygous"
Note: The links to Google Translate in these articles include an icon that will allow you to hear the Greek or Latin pronunciation of the word.
- Details
- Written by: Prof. Claudio R. Molina, MSc
This article was written by Claudio Rodrigo Molina, Josefa Catalán Lobo, and Carolina Becker Fehlandt. We thank them for their contribution to Medical Terminology Daily.
The azygos lobe, also commonly referred to as the" accessory lobe of the azygos vein", was first described in 1877 by Heinrich Wrisberg. It is seen in 0,4 % of chest X-rays; 1,5% in high resolution CT, and 1% in anatomical dissections. It is not a true accessory pulmonary lobe as it does not have its own bronchus and does not correspond to a specific bronchopulmonary segment, the “azygos lobe”, is located at the apicomedial portion of the upper right lobe and it separated from the remainder of the upper lobe by a fissure (Denega et al, 2015; Özdemir et al, 2017)
A convex-shaped fissure is created by the course of the vein bearing towards the medial side of the right lung to join with the superior vena cava. Its formation is a result of an unusual embryogenic migration of the posterior cardinal vein; which is a precursor of the azygos vein (Denega et al, 2015).
Instead of sliding over the lung medially, the vein invaginates into the parenchyma of the lung and becomes enveloped by layer of pleural folds, forming a mesentery-like structure, also called “mesoazygos”. Further migration into the lung as it passes towards the right hilum creates a convex semicircular fissure with the vein located at the base of the fissure. This fissure can be identified in an X-ray chest image as a coma-shaped (“Teardrop sign”) or curved linear shadow in the paramediastinal region of the right lung; it terminates at the level of second costal cartilage (Akhtar et al, 2018; Caceres et al, 1993). The lower portion of the azygos fissure is teardrop-shaped and its contains the azygos vein (Özdemir et al, 2017; Kotovet al, 2017).
Instead of sliding over the lung medially, the vein invaginates into the parenchyma of the lung and becomes enveloped by layer of pleural folds, forming a mesentery-like structure, also called “mesoazygos”. Further migration into the lung as it passes towards the right hilum creates a convex semicircular fissure with the vein located at the base of the fissure. This fissure can be identified in an X-ray chest image as a coma-shaped (“Teardrop sign”) or curved linear shadow in the paramediastinal region of the right lung; it terminates at the level of second costal cartilage (Akhtar et al, 2018; Caceres et al, 1993). The lower portion of the azygos fissure is teardrop-shaped and its contains the azygos vein (Özdemir et al, 2017; Kotovet al, 2017).

Images provided by the authors.
Click on the image for a larger depiction
The pathway of the vein within the lung is subject to individual variation, and this defines the position of the fissure within the apex of the upper lobe. The most superior portion of the fissure adopts a triangular form, called the trigone. The localization of the trigone determinates the size of the azygos lobe (Caceres et al, 1993; Fuad & Mubarak, 2016 ). A Left azygos lobe has been reported, but it is extremely rare (Özdemir et al, 2017)
Diagnosis of the azygos lobe may be complicated by morphologic variants of the fissure, physiological changes in the size of vein, and the projection of additional shadows within the lobe which may be misinterpreted as scar tissue, a calcified area of a post-infection process, or a malignant tissue or nodule.
It usually has no clinical implications and is an incidental finding in images but the azygos vein may undergo physiological variations, reflected by changes in the size of its shadow and its position in the imaging studies. Expiration, the Valsalva maneuver, or the upright position effect on the venous return to the heart, may enhance the size of the vein and its shadow. Changes in intrathoracic pressure may result in the “empty azygos fissure” phenomenon, in which the medial displacement of the azygos vein occurs after the reexpansion of the collapsed lung, secondary to pneumothorax or pleural effusion as well as a shortened mesoazygos.
In rare cases the azygos veins may undergo variceal changes that are usually located in the arc of the vein. They remained asymptomatic or may be accompanied by a “pressure like” or “tightness” sensation within the chest, recurrent hemoptysis with bright red blood dry cough and dyspnea. The initial differential diagnosis includes acute myocardial infarction, aortic dissection and myocarditis. On the chest X-ray it may present as a round or oval paratracheal shadow with a smooth surface or outline. Untreated, it may predispose the patient to the risk of rupture, thrombosis, or pulmonary embolism. Azygos thrombosis is extremely rare and most cases in the literature had an undelaying azygos dilation or some prothrombotic status like malignancy. In all lung tissue some pathological process can originate in the azygos lobe as bullous, bronchiectatic changes, pneumonia and tuberculosis. (Kotov et al, 2018; Denega et al, 2015)
Otherwise, it seems the mesoazygos fold serve as a barrier to dissemination of the infection or malignant cells.
For thoracoscopic procedures, recognition of the azygos lobe is particularly important as it can cause partial obstruction of the surgical site view during thoracoscopic sympathectomy. In the literature, two cases have been reported where the phrenic nerve was coursing within the azygos fissure (Kauffman et al, 2010; Pradhan, 2017; Özdemir et al, 2017; Paul, Siba & James, 2018)
Thoracic surgeons as well as treating physicians need to be aware of this rare anatomical variation.
NOTE: For an explanation of the etymology of the word "azygos" click here.
Sources:
1. Akhtar, Jamal & Lal, Amos & B. Martin, Kevin & Popkin, Joel. (2018). Azygos lobe: A rare cause of right paratracheal opacity. Respiratory Medicine Case Reports. 23. 10.1016/j.rmcr.2018.02.001.
2. Caceres, Jennelyn & Mata, Jonathan & Alegret, X & Palmer, J & Franquet, T. (1993). Increased density of the azygos lobe on frontal chest radiographs simulating disease: CT findings in seven patients. AJR. American journal of roentgenology. 160. 245-8. 10.2214/ajr.160.2.8424325.
3. Denega T, Alkul S, Islam E, Alalawi R. (2015). Recurrent hemoptysis - a complication associated with an azygos lobe. The Southwest Respiratory and Critical Care Chronicles, [S.l.], v. 3, n. 11, p. 44-47. ISSN 2325-9205.
4. Fuad, A.R., & Mubarak (2016). Two Cases of Azygos Lobe with Normal and Aneurysmal Azygos Vein on Computed Tomography. Int J Anat Res 2016, Vol 4(1):1843-45. ISSN 2321-4287
5. Kauffman, Paulo & Wolosker, Nelson & De Campos, José Ribas & Yazbek, Guilherme & Biscegli Jatene, Fábio. (2010). Azygos Lobe: A Difficulty in Video-Assisted Thoracic Sympathectomy. The Annals of thoracic surgery. 89. e57-9. 10.1016/j.athoracsur.2010.03.030.
6.Kotov G, Dimitrova I N, Iliev A, et al. (2018). A Rare Case of an Azygos Lobe in the Right Lung of a 40-year-old Male. Cureus 10(6): e2780. doi:10.7759/cureus.2780
- Details
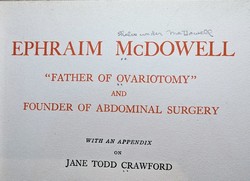
This article is part of the series "A Moment in History" where we honor those who have contributed to the growth of medical knowledge in the areas of anatomy, medicine, surgery, and medical research.
Thomas Dent Mutter was born on March 9, 1811, in Richmond, VA. His mother died in 1813, and his father died of tuberculosis in 1817. Thomas was orphaned when he was barely 8 years old. His father left him a somewhat meager inheritance and in his early life had to do with less that others with his objectives in life. He was well educated under the tutelage of Robert Carter, his guardian, and in 1824 he started his studies at the Hampden Sidney College of Virginia. He continued with a medical apprenticeship with a Dr. Simms in VA. He was well respected and even at his early age he would do home visits for his medical benefactor with great results. He started medical studies at the University of Pennsylvania, where he earned his MD in 1831. The new young doctor, Thomas Dent Mutter, MD was only 20 years of age.
At the time, Europe was the place to go to if you wanted advanced medical studies. Dr. Mutter had no money, so he applied as a ship surgeon to be able to cross the Atlantic. Once in Europe, he spent time in Paris, where he studied under the tutelage of Dr. Guillaume Dupuytren. He later studied for a short time in England where he met Dr. Robert Liston. Following Dupuytren's teachings, Mutter was fascinated by plastic surgery.
A chance encounter with what was to become his first well-known acquisition of a medical curiosity, Mutter started thinking on how to help those people that were known at that time as “monsters”, patients who the general public did not see, because they did not appear in public. The curiosity in question was a wax reproduction of the face of a French woman who had a “horn” arising from her forehead. This piece is on exhibit at the Mütter Museum.
Back in the United States in 1832, Thomas Dent Mutter changed his last name to give it a more “European” sound and added an “umlaut”, so now he was Thomas D. Mütter, MD. It may also be that he wanted to pay homage to his Scottish-German heritage, who knows? He opened his medical office in Philadelphia and although it took time, eventually he had a thriving practice. One of his specialties was the work on “deformities” so common at the time because of facial scars born out of the use of open fires in houses, and deformities caused by burns and loss of tissue due to chemicals used in local industry. Dr. Mütter is the pioneer of what we call today “Reconstructive Surgery”.
In 1835 he was asked to join the Medical Institute of Philadelphia as an assistant professor of Surgery. He was an instant success. Dr. Mütter was adored by his students because, he would question the students and guide them to discovery instead of just lecturing and leaving. In his Discourse eulogy of Dr. Mütter by Joseph Pancoast he writes:” The power of attracting students near him by his mingled gentleness, energy, and enthusiasm; of fixing their attention by the lucid and methodical arrangements of his Subject, by his clear demonstrations, and sprightly oral elucidations, came so readily to him, and was so early displayed) as to seem almost intuitive.” In 1841 Dr Mütter was appointed Professor of Surgery at the Jefferson Medical College in Philadelphia.
Dr. Mütter had always had poor health, even in childhood, and his dedication to his passion, long hours, took its toll on his body.
In 1956 he set sail for Europe and resigned his teaching duties. He was named Emeritus Professor of Surgery. Unfortunately, the trip did not help, and he returned to the US in early 1958. Fearful of another winter in cold Philadelphia, he moved to Charleston, SC, where he died on March 19, 1859.
Dr. Mütter’s story does not end here. He was an avid collector and throughout his short life he had pulled together an impressive collection of medical oddities, samples, and curiosities. Knowing that his life was at an end, he negotiated with the Philadelphia College of Physicians to have them host his collection in perpetuity as well as the creation of a trust fund that would ensure that the public and medical students would have access to this incredible collection. Through the years this collection has increased and is known today as the Mütter Museum of the Philadelphia College of Physicians. I strongly urge our readers to visit this incredible museum. For more information, click here.
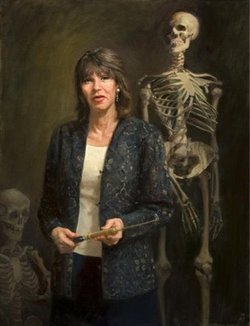
Personal notes: In the late 90’s, I attended a meeting of the American Association of Clinical Anatomists. During the meeting I met Gretchen Worden, who at the time was the Curator of the Mütter museum. Gretchen was inspirational, fun, and a great conversationalist! I had the opportunity to visit Gretchen at the Mütter museum and had the luck to be treated to a “behind the scenes” tour. What an experience! I was saddened to hear that Gretchen Worden passed on August 2, 2004. Still, in my recent visit to the Mütter Museum, I was glad to see a new section at the museum that remembers Gretchen. Her biography can be read here.
I would like to thank Dr. Leslie Wolf for lending me the book by O’Keefe that lead to me writing this article. Dr. Miranda
Sources:
1. “Dr. Mütter’s Marvels: A True Tale of Intrigue and Innovation at the Dawn of Modern Medicine” O’Keefe, C. 2015 Penguin Random House, LLC
2. “A Discourse Commemorative of the Late Professor T.D. Mütter” Pancoast, J. 1859 J Wilson Publisher
3. “Thomas Dent Mütter: the humble narrative of a surgeon, teacher, and curious collector” Baker, J, et al. The American Surgeon, Atlanta 77:iss5 662-14
4. “Thomas Dent Mutter, MD: early reparative surgeon” Harris, ES; Morgan, RF. Ann Plast Surg 1994 33(3):333-8 5.
5 "Things I Learned from Thomas Dent Mütter” O’Keefe C.
All images with permission from The Mutter Museum.
IN MEMORIAM
- Details

Surface anatomy art by Danny Quirk - with permission
UPDATED: Surface anatomy is a subset of human anatomy that studies the relationship of external anatomical landmarks and deeply situated structures. These landmarks are created by cartilage, bones, tendons and muscles. In some cases they may be caused by a hypertrophic or diseased organ. Palpation is and art and my favorite book on the subject is the "Trail Guide to the Body" series by Andrew Biel
Surface anatomy is a core clinical skill for physicians, physical therapists and other health care professionals (HCP), as palpation in specific locations can lead to rapid diagnosis in certain cases. It is also used in surgery to determine the appropriate place for incisions or insertion of a trocar in the case of minimally invasive surgery.
It is true that individual habitus and anatomical variations must make the HCP wary of potential mistakes, but in the majority of cases these anatomical landmarks and diagnoses are correct.
Many book chapters have been written on the topic, but unfortunately, the need to dedicate time to modern discoveries have reduced the time spent on this wonderful learning tool to the point that modern books of anatomy barely touch upon the subject. Many feel today that the need for this tool has been made irrelevant by the bed-side availability of ultrasound imaging. I have to agree with Standring (2012) when she states “I am not convinced that surface anatomy is under growing threat from modern imaging technology…” There is and always will be the need for applied surface anatomy, although maybe not in the way and depth it was used in the past when imaging technology was scarce and expensive.
In order to make the importance of surface anatomy relevant in medical schools, some have added body painting as a tool in their anatomical curriculum with great results. Will it be used everywhere? I doubt it, but here again is a link between human anatomy and art, which our contributor Pascale Pollier presents through her art in "Artem Medicalis".
The artwork in this article is by Danny Quirk. Click on the image for a larger depiction. The video links are for the RMIT University Muscle Man and the Skeletal Man body paintings from the class by Dr. Claudia Diaz.
Personal note: One of the best book chapters on Surface Anatomy was written in "The Anatomical Basis of Clinical Practice" by Becker, Wilson and Gehweiler (1971). Unfortunately, although the content is very good, the images used, the tongue-in-cheek humor, and writing style used by the authors, plus the times at which the book was published forced the publisher stop the sales of this book. It was banned from use in medical colleges through the country. Known to many as the "green book" because of its cover, it is today considered a collector's curiosity. In the "sources" section of this article you can find a links to a journal article on the subject as well as images of the book. Dr. Miranda.
Sources:
1. “Evidence-Based Surface Anatomy” Standrig, S J Clin Anat (2012) 25:813–815
2. “Giving Color to a New Curriculum: Body paint as a Tool in Medical Education” Den Akker, JW. Et al J Clin Anat (2002) 15:356–362
3. “Body-Painting: A Tool Which Can Be Used to Teach Surface Anatomy” Nanjundaiah, K. J Clin Diag Res (2012) October, Vol-6(8): 1405-1408 Copy of the article here
4. “RMIT students paint anatomical man into human textbook” RMIT Dr. Diaz, C. Copy of the article here
5. “Should We Use Body Painting to Teach Anatomy?” Gambino, M article at Smithsonian.com
6. “The role of Fresh Tissue Dissection and Anatomic Body Painting in Anatomy Education” Bennet, C. PPT presentation on PDF here
7. " The anatomical Basis of Medical Practice" Becker, RF. Wilson, JW, Gehweiler, JA 1971, Baltimore, Williams & Wilkins
8. "The Pornographic Anatomy Book? The Curious Tale of The Anatomical Basis of Medical Practice" Halperin EC, Acad Med (2009) 84:2; 278-283 Article here
9. "The Objectification of Female Surface Anatomy" Ruiz, V. Internet article. Click here