Medical Terminology Daily (MTD) is a blog sponsored by Clinical Anatomy Associates, Inc. as a service to the medical community. We post anatomical, medical or surgical terms, their meaning and usage, as well as biographical notes on anatomists, surgeons, and researchers through the ages. Be warned that some of the images used depict human anatomical specimens.
You are welcome to submit questions and suggestions using our "Contact Us" form. The information on this blog follows the terms on our "Privacy and Security Statement" and cannot be construed as medical guidance or instructions for treatment.
We have 526 guests and no members online

Jean George Bachmann
(1877 – 1959)
French physician–physiologist whose experimental work in the early twentieth century provided the first clear functional description of a preferential interatrial conduction pathway. This structure, eponymically named “Bachmann’s bundle”, plays a central role in normal atrial activation and in the pathophysiology of interatrial block and atrial arrhythmias.
As a young man, Bachmann served as a merchant sailor, crossing the Atlantic multiple times. He emigrated to the United States in 1902 and earned his medical degree at the top of his class from Jefferson Medical College in Philadelphia in 1907. He stayed at this Medical College as a demonstrator and physiologist. In 1910, he joined Emory University in Atlanta. Between 1917 -1918 he served as a medical officer in the US Army. He retired from Emory in 1947 and continued his private medical practice until his death in 1959.
On the personal side, Bachmann was a man of many talents: a polyglot, he was fluent in German, French, Spanish and English. He was a chef in his own right and occasionally worked as a chef in international hotels. In fact, he paid his tuition at Jefferson Medical College, working both as a chef and as a language tutor.
The intrinsic cardiac conduction system was a major focus of cardiovascular research in the late nineteenth and early twentieth centuries. The atrioventricular (AV) node was discovered and described by Sunao Tawara and Karl Albert Aschoff in 1906, and the sinoatrial node by Arthur Keith and Martin Flack in 1907.
While the connections that distribute the electrical impulse from the AV node to the ventricles were known through the works of Wilhelm His Jr, in 1893 and Jan Evangelista Purkinje in 1839, the mechanism by which electrical impulses spread between the atria remained uncertain.
In 1916 Bachmann published a paper titled “The Inter-Auricular Time Interval” in the American Journal of Physiology. Bachmann measured activation times between the right and left atria and demonstrated that interruption of a distinct anterior interatrial muscular band resulted in delayed left atrial activation. He concluded that this band constituted the principal route for rapid interatrial conduction.
Subsequent anatomical and electrophysiological studies confirmed the importance of the structure described by Bachmann, which came to bear his name. Bachmann’s bundle is now recognized as a key determinant of atrial activation patterns, and its dysfunction is associated with interatrial block, atrial fibrillation, and abnormal P-wave morphology. His work remains foundational in both basic cardiac anatomy and clinical electrophysiology.
Sources and references
1. Bachmann G. “The inter-auricular time interval”. Am J Physiol. 1916;41:309–320.
2. Hurst JW. “Profiles in Cardiology: Jean George Bachmann (1877–1959)”. Clin Cardiol. 1987;10:185–187.
3. Lemery R, Guiraudon G, Veinot JP. “Anatomic description of Bachmann’s bundle and its relation to the atrial septum”. Am J Cardiol. 2003;91:148–152.
4. "Remembering the canonical discoverers of the core components of the mammalian cardiac conduction system: Keith and Flack, Aschoff and Tawara, His, and Purkinje" Icilio Cavero and Henry Holzgrefe Advances in Physiology Education 2022 46:4, 549-579.
5. Knol WG, de Vos CB, Crijns HJGM, et al. “The Bachmann bundle and interatrial conduction” Heart Rhythm. 2019;16:127–133.
6. “Iatrogenic biatrial flutter. The role of the Bachmann’s bundle” Constán E.; García F., Linde, A.. Complejo Hospitalario de Jaén, Jaén. Spain
7. Keith A, Flack M. The form and nature of the muscular connections between the primary divisions of the vertebrate heart. J Anat Physiol 41: 172–189, 1907.
"Clinical Anatomy Associates, Inc., and the contributors of "Medical Terminology Daily" wish to thank all individuals who donate their bodies and tissues for the advancement of education and research”.
Click here for more information
- Details
UPDATED: [Pes anserinus] is the name given to a tri-flanged structure formed by the attachment of the flattened tendons of three muscles to the anteromedial surface of the superior aspect of the shaft of the tibia. The tendons correspond to the sartorius, the gracilis, and the semitendinosus muscles. The pes anserinus is related superficially to the the tibial insertion of the medial collateral ligament of the knee.
There is a bursa deep to these tendons, the [bursa anserinus], which can be the cause of painful bursitis.
The term [pes anserinus] literally means “goose foot”, as early anatomists compared this structure to the foot of this bird. In Latin [pes] means “foot”, and [anserinus] or [anser] means “goose”.
For other anatomical structures whose names are related to birds, click here.
Thanks to Jackie Miranda-Klein for suggesting this post. Jackie is studying for the Physician Assistant Master's degree at Kettering College. Dr. Miranda.
Image modified from the original: "3D Human Anatomy: Regional Edition DVD-ROM." Courtesy of Primal Pictures
- Details
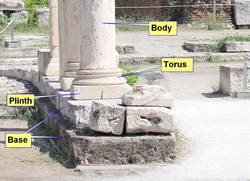
The word [torus] is of Latin origin and refers to “a rounded protuberance or swelling”. In science, it refers to a doughnut-shaped structure (see image). It also refers to the rounded, bulging, and circular base component of a pillar, found between the square plinth and the main body of the pillar. The torus can be seen in Egyptian, Greek, and Roman style pillars.
The term is used in anatomy and medicine to denote normal or abnormal circular or semicircular protuberances, as in the case of the “torus tubarius”, a normal semicircular elevation found at the ostium of the auditory tube (of Eustachius) in the lateral walls of the rhinopharynx. The torus tubarius elevation is due to the presence of lymphoid tissue which can get inflamed.
Torus mandibularis. An exostosis that develops on the inner side of the mandible
Torus palatinus: a benign, small exostosis that appears in the midline of the hard palate
In orthopedics it is used to denote a compression fracture where the cortex of a long bone close to one of its epiphyses buckles under longitudinal (axial) compression. The look of the fracture is similar to the location of the torus in a pillar. An example of this is the torus fracture (also known as buckle fractures) in children.
The term [torulus] is related to [torus], as it means a “small torus” and it refers to a small elevation, which is synonymous with the word “papilla”. An example of this is the term torulus tactiles palmaris, referring to small elevations on the palms of the hand. Another related term is [torulosis], referring to a large number of small elevations or pimples.
The following images are of a Greek pillar taken in 2014 in Athens showing the location of the torus. The next image shows a torus fracture. The image is from www.kidsfractures.com/forearm/ and we thank them for sharing the image with us. This is a great site for information on fractures in children.
Sources:
1. “Medical Meanings: A Glossary of Word Origins” Haubrich, WS. Am Coll Phys. Philadelphia 1997
2. “The Origin of Medical Terms” Skinner, HA 1970, New York. Hafner Publishing Company
3. “Taber’s Cyclopedic Medical Dictionary” 16th Ed. 1989. Philadelphia. FA Davis Company
4. www.kidsfractures.com/forearm/
Torus image: By LucasVB [Public domain], via Wikimedia Commons
Thanks to Jackie Miranda-Klein for suggesting this post. Dr. Miranda.
- Details

Excised bicuspid aortic leaflets
The normal components of the aortic valve are part of the aortic root. The valve is composed of three leaflets, each of which are related to a sinus of Valsalva, and three interleaflet triangles. The anatomy of the aortic root, the aortic valve and the interleaflet triangles of the aortic root have been described in other articles in this website.
A bicuspid aortic valve (BAV) is probably the most common cardiac defect of congenital origin. The prevalence of BAV ranges from 0.9% to 2% in the general population with a 3:1 male-female ratio.
In spite of the anomaly, a BAV may achieve normal valvular function, but this probably does not last, as BAV tend to develop calcifications in the adult leading to valvular disease, dysfunction, valvar stenosis, so complications are common, the most common being dilation of the aortic root and ascending aorta.
The etiology of a BAV is commonly accepted as congenital and there are some studies that demonstrate a familial component, but it can appear in families where there is no known history of BAV.
There are several attempts at classifying BAV, as the leaflets that fuse are different, and so is the way of fusion.
There is one rare BAV called “pure”. This purely BAV is a true BAV, composed of two leaflets of similar size where there is no clear fusion line or “raphe” between the fused leaflets (see image). This valve has two well developed interleaflet triangles and the third can be absent or vestigial. The image depicts the excised calcified leaflets where the left and right coronary cusps are fused.
Other types of BAV have a well-developed raphe, have two well developed interleaflet triangles and the third may be large or anomalous. The leaflets may also be asymmetrical. The classification of the different types of BAV goes beyond the objective of this article, but they can be studied in the references at the end of this article. There is no doubt that the different types of BAV can cause valvar disease and hemodynamic chaos, so the surgical approach for these may be different, including valve repair, aortic annuloplasty, interleaflet triangle remodeling, and of course valve removal and prosthetic implant, either biological or mechanical.
Clinically, the pathologies related to the function of the aortic valve are stenosis, valvular incompetence, and in some cases intimal aortic dissection, which is a catastrophic complication. Some of these complications are triggered by the calcification of the bicuspid leaflets. Interestingly, although BAV is a congenital disease, only one in fifty children known to have BAV have clinically significant disease by adolescence.
PERSONAL NOTE: I have permission to publish the image in this article… because the bicuspid aortic valve depicted in this article is my own. My personal thanks to the medical and support personnel at the Memorial Hermann Heart & Vascular Institute, in Houston, TX., and my three cardiovascular physicians without whom I would not be back writing this article, Drs. Randall K. Wolf (contributor to this website), Dr. William Ross Brown (cardiologist), and Dr. Tuyen (Tom) Nguyen, who operated on me. Dr. Miranda.
Sources:
1. “Etiology of bicuspid aortic valve disease: Focus on hemodynamics: Atkins, SA, Sucosky, P World J Cardiol. 2014 Dec 26; 6(12): 1227–1233.
2. “A classification system for the bicuspid aortic valve from 304 surgical specimens” Sievers, HH., Schmidtke, C. J Thorac Cardiovasc Surg 2007;133:1226-33
3. “Bicuspid Aortic Valve Disease” Siu, SC, Silversides, CK. JACC Vol. 55, No. 25, 2010:2789 – 800
4. “Bicuspid aortic valve aortopathy in adults: Incidence, etiology, and clinical significance” Int J Card 2015:1;400-407
5. ”Sutureless valve in freestyle root: new surgical valve-in-valve therapy” Villa E, Messina A et al. Ann Thorac Surg 2013:96:e155–e157
6.” Sutureless aortic bioprosthesis valve implantation and bicuspid valve anatomy: an unsolved dilemma?” Lona, M, Guichard JB, et al Heart vessels 2016.31:1783-1789
- Details
- Written by: Efrain A. Miranda, Ph.D.
- Hits: 141283
This is the most popular article on this blog by far! Look at the hits counter above...
Let us know other topics that may interest you in our "Contact Us" page.
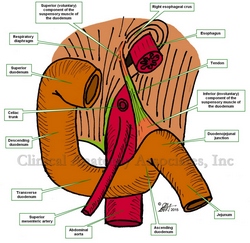
The ligament of Treitz is formed by a fold of peritoneum over the suspensory muscle of the duodenum. This muscle is also known as the "muscle of Treitz" or "musculus suspensorius duodenii". It was first described in 1853 by Dr. Václav Treitz.
The muscle (see the first image) has an unusual structure in that it is formed by a tendon with two muscular ends of dissimilar embryological origin and function. The superior muscular component is skeletal (voluntary) muscle and arises as a slip of muscle (Hilfsmuskel) from the right esophageal crus of the respiratory diaphragm, as well as muscular and ligamentous fibers arising in the region of origin of the celiac trunk and superior mesenteric artery. The inferior portion of the muscle is smooth (involuntary) muscle and has been described as continuous with both the longitudinal and circular muscle layers of the intestine at the duodenojejunal junction.
The ligament of Treitz is an anatomical landmark used by anatomists and surgeons to denote the duodenojejunal junction and the point where the small intestine passes from retroperitoneal duodenum to intraperitoneal jeunum. Surgeons use the ligament of Treitz to measure the jejunum to decide where to perform an anastomosis.
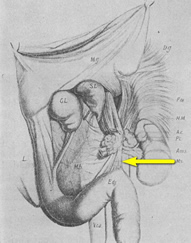
Original image of the "ligament of Treiz"
There is much discussion today on eponyms, that is, associating an individual's name to an anatomical structure or surgical procedure. In spite of the pressure to make eponyms dissapear, the ligament of Treitz is here to stay!
The second image is a copy of the original image published by Dr. Václav Treitz in his 1853 publication "Ueber einen neuen Muskel am Duodenum des Menschens" (On a new muscle in the duodenum of man). The 'muscle of Treitz" is marked by an arrow.
It is important to clarify that the term "ligament" in the abdominopelvic cavity has a different meaning and structure from a skeletal ligament found in a joint. For more information click here. The term "Ligament of Treitz" refers to the fold of peritoneum that attaches to the posterior aspect of the abdominal and lines the "muscle of Treitz".
Clinical anatomy, pathology, and surgery of the gastrointestinal tract are some of the many lecture topics developed and delivered to the medical devices industry by Clinical Anatomy Associates, Inc.
Sources:
1. "Clinically Oriented Anatomy" Moore, KL. 3r Ed. Williams & Wilkins 1992
2. "The origin of Medical Terms" Skinner, AH, 1970
3. "The suspensory muscle of the duodenum and its nerve supply" Jit, I.; Singh, S. J. Anat. (1977), 123, 2, pp. 397-405
4. "Anatomical and functional aspects of the human suspensory muscle of the duodenum." Costacurta, L. Acta Anat (Basel). 1972;82(1):34-46
Image property of: CAA.Inc. Artists: Dr. E. Miranda and D.M. Klein
- Details
- Written by: Efrain A. Miranda, Ph.D.
Interleaflet triangles of the aortic valve by MTD.
Click for a larger image.
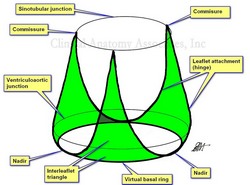
The interleaflet triangles (ILTs) are three triangular regions found in the ventricular aspect of the aortic root. They are bound inferiorly by the virtual basal ring (VBR), laterally by the attachment of the leaflets (the hinge) to the aorta and left ventricular wall (muscular and fibrous), and superiorly by the commissures (site of attachment and meeting of adjacent leaflets) which are usually located at the sinotubular junction, also known as the sinotubular ridge.
A review of the literature on the topic shows that although many speak of these ILTs, not many authors have clearly defined their boundaries. In fact, some only reserve the term ILT to the triangular region distal to the ventriculoaortic boundary. The description used in this article includes the ventricular wall found between the VBR and the ventriculoaortic junction as well as fibrous components found between these two boundaries. Based on this description, we have developed an image of the ILTs that, to our knowledge is not found in literature. (see accompanying images).
The virtual basal ring is a circular virtual line formed by the nadirs of the three aortic leaflets (cusps). The attachment of the three leaflets create a three-pronged coronet that is useful in defining the interleaflet triangles (see image)
The superior boundary of the ILTs is formed by three commissures, the points where the leaflets meet each other at the sinotubular junction. There are two posterior commissures, right and left. The right-posterior commissure is found between the noncoronary and the left coronary sinuses (of Valsalva). An important point about this commissure is that it is situated above the midpoint of the septal (anterior) leaflet of the mitral valve. The left-posterior commissure is found between the left and the right coronary sinuses. The anterior commissure is located between the right and the noncoronary sinus close to the membranous interventricular septum.
Based on the above description, there are three interleaflet triangles:
a. Right (posterior), left (posterior), and anterior. The right posterior ILT is located between the noncoronary and the left coronary sinuses, and just as the commissure at its apex, is located at the midpoint of the septal (anterior) leaflet of the mitral valve. Also, the superior aspect of this ILT is related to the transverse pericardial sinus.
b. The left posterior ILT is located between the right and the left coronary sinuses, and is lies immediately behind the right ventricular outlet.
c. The anterior ILT is found between the right and the noncoronary sinuses. It is related to the membranous septum and the right fibrous trigone, forming part of the central fibrous body (skeleton) of the heart. This ILT is a good anatomical landmark to the location of the bundle of His and the left bundle branch, both components of the conduction system of the heart. These structures can be compressed during the implantation of an aortic or mitral valve, causing transitory or permanent cardiac conduction problems.
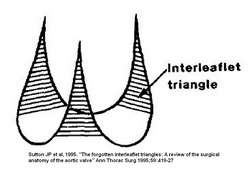
Interleaflet triangles of the aortic valve by Sutton.
Click for a larger image.
The ILTs are important in the normal physiology and hemodynamics of the aortic valve. A small ILT will affect the diameter of the valve and the movement of the leaflets, causing stenosis. This is the case in bicuspid aortic valves where the fusion of two of the leaflets leads to the reduction in size of the ILT normally found between these two fused leaflets.
Since they are located within the functional portion of the left ventricle, the ILTs are subject to the pressures of the ventricle and can be areas that develop aneurysms.
Because of their importance in the hemodynamics of the aortic valve, new procedures and medical devices that reshape the ILTs are being developed. This is specially important in the case of a bicuspid aortic valve, where the interleaflet triangles may be abnormal.
Further to the images that are depicted in this article, the lower image is the classic image of the interleaflet triangles by Sutton (1995). As you can see, the base of the triangles is shown straight with no clear boundary, and it seems as though they are related to the ventriculoaortic junction. The nadirs are not used as a point of reference. The upper image (developed by us and based on Sutton's original sketch) clearly shows the extent of the ILTs as well as their relation to the three landmarks that define the aortic root: The virtual basal ring, the ventriculoaortic junction, and the sinotubular junction.
NOTE: The pulmonary valve also has interleaflet triangles, with a somewhat similar description, but since they are under low pressure they do not develop or are cause of pathology as the ILTs of the aortic valve.
Sources:
1. The Anatomy of the Aortic Root: Loukas, M et al. Clinical Anatomy 27:748–756 (2014)
2. “Extracardiac aneurysm of the interleaflet triangle above the aortic-mitral curtain due to infective endocarditis of the bicuspid aortic valve.” Hori D, et al. Gen Thorac Cardiovasc Surg. 2008 Aug;56(8):424-6
3. “Anatomy of the aortic root: implications for valve-sparing surgery” Efstratios I. Charitos, HS. Ann Cardiothorac Surg 2013;2(1):53-56
4. “The Forgotten Interleaflet Triangles: A Review of the Surgical Anatomy of the Aortic Valve” Sutton JP, et al Ann Thorac Surg 1995;59:419-27
5.” The aortic interleaflet triangles annuloplasty: a multidisciplinary appraisal” Mangini, A., et al. European Journal of Cardio-Thoracic Surgery, Vol. 40:4, 2011, 851-857
6. “Structure and Anatomy of the Aortic Root” Ho, SH., Eur J Electrocar 2009 10; i3-i10
7. “In vitro study of the aortic interleaflet triangle reshaping” Vismara, R Journal of Biomechanics; 47:2; 2014. 329-33
- Details
- Written by: Efrain A. Miranda, Ph.D.
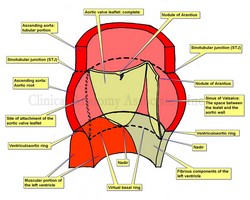
Aortic root and aortic valve.
Click for a larger image.
This article is a continuation of: The aortic root and the aortic valve (1)
The aortic valve is formed by three semilunar leaflets which are very thin as to be almost transparent. The attachment of the leaflets is complex, as part of them attaches to ventricular wall, part attaches to the sinusal arterial wall, and even part of them attaches to the membranous interventricular septum and other fibrous structures. Loukas et al state that at “least one third of the circumference of the aortic root is supported by fibrous tissue rather than ventricular musculature”
Each of the three aortic leaflets has a semilunar attachment and shape (hence the term “semilunar valve” used for both the aortic and pulmonary valve, as they have similar shape). The attachment of these three leaflets create a continuous line where the highest points are the three locations where the leaflets attach at the STJ, and the three lower points or “nadirs” form an edge shaped like a three-pronged “coronet”. This coronet is called by many the “anatomical anulus” of the aortic valve, as this is where the fibrous skeleton of the heart forms the “hinges” of the aortic valve.
The leaflets of the aortic valve (as well as those in the pulmonary valve) have a tissue excrescence that can become quite hard at the point where the three leaflets touch on each heartbeat. These are the nodules of Arantius, named after Giulio Cesare Aranzio (1530 – 1589). As a side note, the nodules of the pulmonary valve have a different name. Distally, the aortic leaflets may present a very thin extension that may be cribriform (not shown in the sketch). These are called the lunulae (singular: lunula) as they look like a sliver of moon.
The second component of the base of the aortic root is a ring defined by the lowest portion of each leaflet, the nadir. This ring is called the “virtual basal ring”, is found within the left ventricle and is used as a surgical reference for aortic valve replacement implants.
The three leaflets are found within three dilations of the aortic root, each one called a “sinus of Valsalva”, which extend between the virtual basal ring inferiorly and the STJ superiorly. The presence of the sinuses of Valsalva permits “fluttering” of the open aortic leaflets in ventricular systole. This fluttering of the leaflets allows blood to flow into the sinuses and into the coronary arteries during ventricular systole.
Aortic valve may present with different number of leaflets, as in the case of a bicuspid aortic valve.
The shape of the attachment of the leaflets create two distinct situations:
First, there is a portion of the ventricle related to the leaflets where the ventricle acts as an artery, the aorta. These areas are found inside the sinuses of Valsalva.
Second, there are triangular areas of the aortic root (the interleaflet triangles) where the aortic wall is within the left ventricle and submitted to the pressures and hemodynamics of the left ventricle. These interleaflet triangles have been involved in aneurysms. For simplicity, these interleaflet triangles are not shown in the sketch and are the subject of a separate article in this website.
Note: The image depicts only one complete aortic leaflet. The other one has been transected to show the sinus of Valsalva and the third has been removed to show the attachment or "hinge" of the leaflet. For an anatomical image of the aortic valve click here.
Sources:
1. The Anatomy of the Aortic Root: Loukas, M et al. Clinical Anatomy 27:748–756 (2014)
2. “Extracardiac aneurysm of the interleaflet triangle above the aortic-mitral curtain due to infective endocarditis of the bicuspid aortic valve.” Hori D, et al. Gen Thorac Cardiovasc Surg. 2008 Aug;56(8):424-6
3. “Anatomy of the aortic root: implications for valve-sparing surgery” Efstratios I. Charitos, HS. Ann Cardiothorac Surg 2013;2(1):53-56
4. “The Forgotten Interleaflet Triangles: A Review of the Surgical Anatomy of the Aortic Valve” Sutton JP, et al Ann Thorac Surg 1995;59:419-27
Image property of: CAA, Inc. Artist: Dr. Miranda

![Torus - By LucasVB [Public domain], via Wikimedia Commons](/images/MTD/SmallImages/torus_sm.jpg)