Medical Terminology Daily (MTD) is a blog sponsored by Clinical Anatomy Associates, Inc. as a service to the medical community. We post anatomical, medical or surgical terms, their meaning and usage, as well as biographical notes on anatomists, surgeons, and researchers through the ages. Be warned that some of the images used depict human anatomical specimens.
You are welcome to submit questions and suggestions using our "Contact Us" form. The information on this blog follows the terms on our "Privacy and Security Statement" and cannot be construed as medical guidance or instructions for treatment.
We have 508 guests and no members online

Jean George Bachmann
(1877 – 1959)
French physician–physiologist whose experimental work in the early twentieth century provided the first clear functional description of a preferential interatrial conduction pathway. This structure, eponymically named “Bachmann’s bundle”, plays a central role in normal atrial activation and in the pathophysiology of interatrial block and atrial arrhythmias.
As a young man, Bachmann served as a merchant sailor, crossing the Atlantic multiple times. He emigrated to the United States in 1902 and earned his medical degree at the top of his class from Jefferson Medical College in Philadelphia in 1907. He stayed at this Medical College as a demonstrator and physiologist. In 1910, he joined Emory University in Atlanta. Between 1917 -1918 he served as a medical officer in the US Army. He retired from Emory in 1947 and continued his private medical practice until his death in 1959.
On the personal side, Bachmann was a man of many talents: a polyglot, he was fluent in German, French, Spanish and English. He was a chef in his own right and occasionally worked as a chef in international hotels. In fact, he paid his tuition at Jefferson Medical College, working both as a chef and as a language tutor.
The intrinsic cardiac conduction system was a major focus of cardiovascular research in the late nineteenth and early twentieth centuries. The atrioventricular (AV) node was discovered and described by Sunao Tawara and Karl Albert Aschoff in 1906, and the sinoatrial node by Arthur Keith and Martin Flack in 1907.
While the connections that distribute the electrical impulse from the AV node to the ventricles were known through the works of Wilhelm His Jr, in 1893 and Jan Evangelista Purkinje in 1839, the mechanism by which electrical impulses spread between the atria remained uncertain.
In 1916 Bachmann published a paper titled “The Inter-Auricular Time Interval” in the American Journal of Physiology. Bachmann measured activation times between the right and left atria and demonstrated that interruption of a distinct anterior interatrial muscular band resulted in delayed left atrial activation. He concluded that this band constituted the principal route for rapid interatrial conduction.
Subsequent anatomical and electrophysiological studies confirmed the importance of the structure described by Bachmann, which came to bear his name. Bachmann’s bundle is now recognized as a key determinant of atrial activation patterns, and its dysfunction is associated with interatrial block, atrial fibrillation, and abnormal P-wave morphology. His work remains foundational in both basic cardiac anatomy and clinical electrophysiology.
Sources and references
1. Bachmann G. “The inter-auricular time interval”. Am J Physiol. 1916;41:309–320.
2. Hurst JW. “Profiles in Cardiology: Jean George Bachmann (1877–1959)”. Clin Cardiol. 1987;10:185–187.
3. Lemery R, Guiraudon G, Veinot JP. “Anatomic description of Bachmann’s bundle and its relation to the atrial septum”. Am J Cardiol. 2003;91:148–152.
4. "Remembering the canonical discoverers of the core components of the mammalian cardiac conduction system: Keith and Flack, Aschoff and Tawara, His, and Purkinje" Icilio Cavero and Henry Holzgrefe Advances in Physiology Education 2022 46:4, 549-579.
5. Knol WG, de Vos CB, Crijns HJGM, et al. “The Bachmann bundle and interatrial conduction” Heart Rhythm. 2019;16:127–133.
6. “Iatrogenic biatrial flutter. The role of the Bachmann’s bundle” Constán E.; García F., Linde, A.. Complejo Hospitalario de Jaén, Jaén. Spain
7. Keith A, Flack M. The form and nature of the muscular connections between the primary divisions of the vertebrate heart. J Anat Physiol 41: 172–189, 1907.
"Clinical Anatomy Associates, Inc., and the contributors of "Medical Terminology Daily" wish to thank all individuals who donate their bodies and tissues for the advancement of education and research”.
Click here for more information
- Details
- Written by: Efrain A. Miranda, Ph.D.
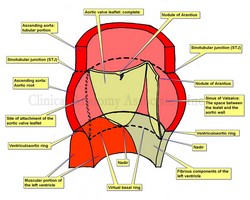
Aortic root and aortic valve.
Click for a larger image.
The term “aortic valve” refers to the three leaflets (or cusps) components that allow passage of blood from the left ventricle to the ascending aorta during ventricular systole, while at the same time preventing regurgitation or reflux of blood back into the ventricle during ventricular diastole. In reality, the “valve” is only a component of a larger structure called the “aortic root”. This article will describe the components of the aortic root and the aortic valve.
The ascending aorta presents with two distinct segments. The proximal segment is a dilated portion called the aortic root. The distal portion is known as the tubular portion of the ascending aorta. The boundary between these two portions is the [sinotubular junction (STJ). Some authors will recognize as the ascending aorta only the tubular portion.
The aortic root is that portion of the ventricular outflow tract and proximal aorta that supports the leaflets of the aortic valve. It is a functioning unit with relations both to the to the aorta and to the left ventricle, and it is here where in most cases we find the ostia of the right and left coronary arteries.
The aortic root is composed of the three dilated sinuses of Valsalva, two of which give origin to the coronary arteries (right and left), three leaflets (or cusps), and the interleaflet triangles. While the distal boundary of the aortic root is clearly defined (the STJ), the proximal boundary is not as clear and is difficult to define. The STJ is defined by the apices of the three aortic leaflets as well as a clear line that appears as the aorta passes from the dilations of the sinuses of Valsalva to the well-defined tubular portion of the ascending aorta.
This proximal boundary is defined clinically by two circular regions: the ventriculoaortic ring distally and the virtual basal ring proximally.
The ventriculoaortic ring is a circular region formed by the left ventriculoaortic junction (the point where the aorta anchors on the left ventricle), and fibrous tissue of both the “cardiac skeleton” and the membranous interventricular septum. It is also called the “surgical anulus”. This is the area where a surgeon will anchor an aortic replacement valve.
Continued here: The Aortic Root and the Aortic Valve (2)
Note: The image depicts only one complete aortic leaflet. The other one has been transected to show the sinus of Valsalva and the third has been removed to show the attachment or "hinge" of the leaflet. For an anatomical image of the aortic valve click here.
Sources:
1. The Anatomy of the Aortic Root: Loukas, M et al. Clinical Anatomy 27:748–756 (2014)
2. “Extracardiac aneurysm of the interleaflet triangle above the aortic-mitral curtain due to infective endocarditis of the bicuspid aortic valve.” Hori D, et al. Gen Thorac Cardiovasc Surg. 2008 Aug;56(8):424-6
3. “Anatomy of the aortic root: implications for valve-sparing surgery” Efstratios I. Charitos, HS. Ann Cardiothorac Surg 2013;2(1):53-56
4. “The Forgotten Interleaflet Triangles: A Review of the Surgical Anatomy of the Aortic Valve” Sutton JP, et al Ann Thorac Surg 1995;59:419-27
Image property of: CAA, Inc. Artist: Dr. Miranda
- Details
- Written by: Efrain A. Miranda, Ph.D.
Andreas Vesalius Bruxellensis (1515-1564) is considered to be the father of modern anatomy, remembered because an illustrious life and by his book “De Humani Corporis Fabrica, Libri Septem” published first in 1543. Scores of books, translations, articles, and analyzes of his work have been published in the over 500 years since his birth.
With such an incredible pedigree we would expect his name to be attached to more than a few anatomical structures, many of which were first described in his opus magnus, the “Fabrica”, I wonder why this is not so. It is true that modern anatomy is trying to move from eponyms to more descriptive anatomical terms. Still, there are many that will not go away, as is the famous ligament of Treitz, or the sphincter or Oddi.
Today there is only one recorded eponym for Andreas Vesalius, the os vesalianum, a rare accessory bone in the foot located proximally to the base of the fifth metatarsal. It is usually asymptomatic, but in rare cases it can cause pain. It is formed by the failed fusion of the secondary ossification center of the fifth metatarsal.
Reviewing history, I was able to find other references to Andreas Vesalius eponyms or potential eponyms, now in disuse or misnamed:
- Suspensory ligaments of the mammary gland. Although first described by Vesalius in the Fabrica, these structures are named after Sir Astley Paston Cooper (1768 -1841), almost 300 years after being described by the great anatomist, who called them a “fleshy membrane” that stretched between the pectoral fascia and the skin.
- The vermiform appendix. Although called by many just “the appendix”, this structure is mentioned, but not named, by Jacobo Berengario da Carpi in 1524. It was Andreas Vesalius who first described it as an appendix, suggested it looked like a worm (Lat: vermis) calling it the “vermiform appendix”.
- The ligamentum suspensorium Vesalii or crural arch. First described by Giovanni Baptista Morgagni (1682-1771), it was named in honor of Vesalius by Dr. Laurentii (Lorenz) Heisters in his “Compendium Anatomicum” published in 1756. Other authors point to Gabrielle Fallopius as the first to describe this structure in 1561, although he did publish later than Vesalius (1543). Although named after Vesalius, it was later named after Francois Poupart who described it in 1695. You probably know this structure as the inguinal ligament.
- The ligamentum teres femoris. The round ligament of the femur was also first described by Vesalius in 1543.
NOTE: If you have other structures that have been named after Vesalius, please let me know by clicking here
Sources:
1. “A Rare Cause of Foot Pain with Golf Swing. Symptomatic Os Vesalianum Pedis—A Case Report” Petrera, M et al. Sports Health. 2013 Jul; 5(4): 357–359.
2. “Andreas Vesalius’ 500th Anniversary: First Description of the Mammary Suspensory Ligaments” Brinkman RJ, Hage, JJ. World J Surg (2016) 40:2144–2148
3. “Compendium Anatomicum” Heisters, L. 1756 (German)
4. “Anatomy: An Encyclopedic Reference to the Language of Anatomy and Neuroanatomy. It Provides the Fascinating Origin of Terms and Biographies of Anatomists/Physicians Who Originated Them” Bergman, RA, Afifi, AK 2016
- Details
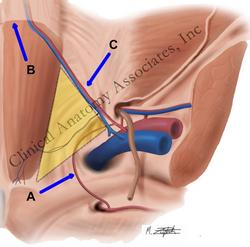
Hesselbach's triangle.
Click for a larger image.
UPDATED: From the Greek [ep(i)] meaning "outer, above, or upon", and the Greek suffix [o-nym] meaning "name". The word [eponym] refers to a person's name becoming attached to an anatomical location or surgical procedure. For centuries it has been the custom to honor or remember someone by attaching their name to a structure, location, procedure, or maneuver.
This has changed as anatomists tend now to give locations and structures descriptive terms. An example of this would be the "Ampulla of Vater" named after the German anatomist Abraham Vater (1684-1751) described today in anatomical texts as the "hepatopancreatic ampulla". The controversy on using eponyms or not goes on...
There are many eponymical terms in the medical arena; following are some of them, click on the links for additional information:
• Hesselbach’s triangle: Named after Franz Kaspar Hesselbach (1759-1816) (see yellow insert in superior image)
• Spigelian line (linea semilunaris): Site for an Spigelian hernia, named after Adrian Van Der Spigelius (1578-1625) (see blue arrow in inferior image)
• Fallopian tube: Named after Gabrielle Fallopius (1523-1563)
• Cooper's pectineal ligament. Named after Sir Astley Paston Cooper (1768-1841)
• Hartmann's procedure: A two-stage colon resection and anastomosis. Named after Prof. Henri Hartmann (1860-1952), a French surgeon.
• Heimlich's maneuver: Named after Dr. Henry J. Heimlich (1920 - 2016)
• Ligament of Treitz: Named after Václav Treitz (1819 - 1872), a Czech pathologist.
• Sphincter of Oddi. Named after Ruggero Oddi (1864 - 1913), an Italian anatomist.
If you want to see a listing of the eponyms in this website, click here.
Here is an article on "The lost influence of Andreas Vesalius on eponymic anatomy".
Here is an interesting article on eponyms by Ilana Yurkiewicz published on 11/15/2012 in Scientific American: "Modern medical terms are still named after Nazi doctors. Can we change it?". It is interesting and thougthful reading.
PERSONAL NOTE: Many anatomists today are actively trying to eliminate eponyms from anatomical, medical, and surgical books. For me, this eliminates the interest of learning about the people who either first described these structures or procedures, which is one of the objectives of this website. I wonder (and this is a tongue-in-cheek comment) if the reason for this desire to eliminate eponyms is because there are so many attached to anatomical structures that there is no place for their own names! When history has forgotten about the original eponyms maybe we will see new ones with the names of modern anatomists! I do not worry, my name is attached to the "Ligaments of Miranda"... don't ask! Dr. Miranda
Superior image property of: CAA.Inc.. Artist: M. Zuptich.
Inferior image property of :CAA.Inc.. Artist:D.M. Klein
- Details
UPDATED: The ascending aorta is the first and most proximal portion of the aorta. About 5 cm. in length and 3 cm. in diameter at its origin, its proximal end begins at the superior aspect of the outflow tract of of the left ventricle, at the ventriculoaortic junction.
The ascending aorta ends superiorly at an imaginary horizontal plane (blue dotted line) that passes through the sternal angle (of Louis), continuing distally with the aortic arch. This is an important anatomical landmark, as many surgeons use as the superior border of the ascending aorta an oblique plane that passes proximal to the brachiocephalic trunk (yellow dotted line). Although this landmark could be useful in surgery, it is not anatomically correct.
Since the sternal angle (of Louis) also indicates the superior border of the pericardial sac, it can be said that the ascending aorta is completely intrapericardial, and in surgery the pericardial sac should be the anatomical landmark used to separate the ascending aorta from the aortic arch.
From its point of origin at the ventriculoaortic junction, the aorta presents with a dilated region where the aortic valve is located. The aortic valve is one of the two semilunar valves of the heart, and the dilation of this region is caused by the presence of the sinuses of Valsalva. This dilated bulbous segment is known as the aortic root.
The dilated, sinus portion, or aortic root segment of the ascending aorta continues superiorly with the tubular portion of the ascending aorta. The area of transition between these two components is marked by a sharp crease known as the sinotubular junction (STJ). The dilation of the aortic root is caused by the presence of the sinuses of Valsalva, named after Antonio Maria Valsalva (1666 - 1723).
The tubular portion of the ascending aorta ascends with an inclination anteriorly and to the right. The ascending aorta presents with a slight anterior bulge causing the transverse section of this aortic segment to be slightly oval.
Only two arteries arise from the ascending aorta, both usually at the aortic root segment, just inferior to the STJ. These are the right coronary artery and the left coronary artery. There are anatomical variations where only one, or up to five different coronary arteries have been described.
At its origin, the aorta presents with semilunar folds of the serous surface of the pericardium. Also known as the ascending aortic folds, or Rindfleisch's folds, these are eponymically named after Georg Eduard Von Rindfleisch (1836 – 1908), a German pathologist and histologist of Bavarian nobility ancestry.
Image property of: CAA.Inc.. Artist: Dr. E. Miranda
- Details
Kernicterus is a disorder where excess bilirubin accumulates in the deep neural tissues of the brain and can cause brain damage in the newborn.
It is characterized by jaundice and a limpness of the newborn, devoid of energy. Can present with seizures, convulsions, and muscle spasms.
This condition is treatable and requires awareness from the parents if yellowness of the skin (jaundice) is detected along with the above-mentioned signs in the early days post-partum. There are other signs not mentioned in this article
The word [kernicterus] comes from the German word [kern], meaning “nucleus” or “core”. In this particular word the term kern refers to the fact that one of the most importantly affected brain structures in kernicterus are the basal nuclei of the brain (wrongly called the "basal ganglia"). It also includes the word [icterus] from the Greek word [ικτερός] pronounced (ikterós). The word [icterus] in Greek was originally used to denote a yellow bird, and is now used to denote the yellow color of jaundice.
We would like to thank diseasepictures.com for the image in this article. For additional information on neonatal jaundice, click here.
Sources:
1. Clayman, L. "The AMA Encyclopedia of Medicine" 1989. Random House, NY
2. “The Origin of Medical Terms” Skinner HA 1970 Hafner Publishing Co.
Thanks to Jackie Miranda-Klein for her contribution suggesting this word.
- Details
The term [parenchyma] is a Greek term (παράένχέω). Its origin and meaning have little relation to the medical use of the term. The word means "that what is poured" or to "pour in". The actual definition of the term is "the proper mass of a solid organ". If someone refers to the "liver parenchyma", they are referring to the hepatic tissue, so it is with any other solid organ.
The etymology of the word is obscure and reflects ancient physiological theories and history. Vesalius mentions that the word was introduced by Erasistratus circa 300BC. He thought that the blood was "poured" into the organ and then this poured fluid would congeal to form the organ's proper mass. With time this concept was abandoned, but the word persisted to its modern meaning.
Interesting, there are many which accentuate the word wrongly. The accent or stress should be on the letter "e" and not on the letter 'y", so it should be pronounced "parénchyma"