Medical Terminology Daily (MTD) is a blog sponsored by Clinical Anatomy Associates, Inc. as a service to the medical community. We post anatomical, medical or surgical terms, their meaning and usage, as well as biographical notes on anatomists, surgeons, and researchers through the ages. Be warned that some of the images used depict human anatomical specimens.
You are welcome to submit questions and suggestions using our "Contact Us" form. The information on this blog follows the terms on our "Privacy and Security Statement" and cannot be construed as medical guidance or instructions for treatment.
We have 941 guests online

Jean George Bachmann
(1877 – 1959)
French physician–physiologist whose experimental work in the early twentieth century provided the first clear functional description of a preferential interatrial conduction pathway. This structure, eponymically named “Bachmann’s bundle”, plays a central role in normal atrial activation and in the pathophysiology of interatrial block and atrial arrhythmias.
As a young man, Bachmann served as a merchant sailor, crossing the Atlantic multiple times. He emigrated to the United States in 1902 and earned his medical degree at the top of his class from Jefferson Medical College in Philadelphia in 1907. He stayed at this Medical College as a demonstrator and physiologist. In 1910, he joined Emory University in Atlanta. Between 1917 -1918 he served as a medical officer in the US Army. He retired from Emory in 1947 and continued his private medical practice until his death in 1959.
On the personal side, Bachmann was a man of many talents: a polyglot, he was fluent in German, French, Spanish and English. He was a chef in his own right and occasionally worked as a chef in international hotels. In fact, he paid his tuition at Jefferson Medical College, working both as a chef and as a language tutor.
The intrinsic cardiac conduction system was a major focus of cardiovascular research in the late nineteenth and early twentieth centuries. The atrioventricular (AV) node was discovered and described by Sunao Tawara and Karl Albert Aschoff in 1906, and the sinoatrial node by Arthur Keith and Martin Flack in 1907.
While the connections that distribute the electrical impulse from the AV node to the ventricles were known through the works of Wilhelm His Jr, in 1893 and Jan Evangelista Purkinje in 1839, the mechanism by which electrical impulses spread between the atria remained uncertain.
In 1916 Bachmann published a paper titled “The Inter-Auricular Time Interval” in the American Journal of Physiology. Bachmann measured activation times between the right and left atria and demonstrated that interruption of a distinct anterior interatrial muscular band resulted in delayed left atrial activation. He concluded that this band constituted the principal route for rapid interatrial conduction.
Subsequent anatomical and electrophysiological studies confirmed the importance of the structure described by Bachmann, which came to bear his name. Bachmann’s bundle is now recognized as a key determinant of atrial activation patterns, and its dysfunction is associated with interatrial block, atrial fibrillation, and abnormal P-wave morphology. His work remains foundational in both basic cardiac anatomy and clinical electrophysiology.
Sources and references
1. Bachmann G. “The inter-auricular time interval”. Am J Physiol. 1916;41:309–320.
2. Hurst JW. “Profiles in Cardiology: Jean George Bachmann (1877–1959)”. Clin Cardiol. 1987;10:185–187.
3. Lemery R, Guiraudon G, Veinot JP. “Anatomic description of Bachmann’s bundle and its relation to the atrial septum”. Am J Cardiol. 2003;91:148–152.
4. "Remembering the canonical discoverers of the core components of the mammalian cardiac conduction system: Keith and Flack, Aschoff and Tawara, His, and Purkinje" Icilio Cavero and Henry Holzgrefe Advances in Physiology Education 2022 46:4, 549-579.
5. Knol WG, de Vos CB, Crijns HJGM, et al. “The Bachmann bundle and interatrial conduction” Heart Rhythm. 2019;16:127–133.
6. “Iatrogenic biatrial flutter. The role of the Bachmann’s bundle” Constán E.; García F., Linde, A.. Complejo Hospitalario de Jaén, Jaén. Spain
7. Keith A, Flack M. The form and nature of the muscular connections between the primary divisions of the vertebrate heart. J Anat Physiol 41: 172–189, 1907.
"Clinical Anatomy Associates, Inc., and the contributors of "Medical Terminology Daily" wish to thank all individuals who donate their bodies and tissues for the advancement of education and research”.
Click here for more information
- Details
The root term [-dext-] and its variant [-dexter-] arise from the Latin [dexter] meaning "right". It may be pointed out that the modern Greek word for "right" is [δεξιά] (dexia), and they are probably related with the Latin term.
It is interesting that a word meaning "right" would be used in the word "dexterous" meaning "skilled". The reason is that the right hand, being the one most used by many is more skilled than the left hand.
The term [ambidextrous] is said to mean "someone skilled with both hands". In reality, it refers to a person that "has two right hands", therefore skilled with both hands.
- Details
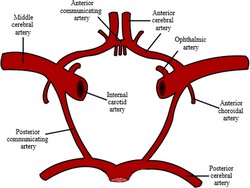
The middle cerebral arteries are paired terminal branches of the internal carotid artery. Each middle cerebral artery supplies arterial blood to the brain beyond the arterial circle of Willis. The vascular territory of the middle cerebral artery supplies the lateral surfaces of the frontal, parietal, and temporal cerebral lobes as well as the deeply situated insular lobe.
There are many anatomical variations of the middle cerebral artery, as described here.
Clinical anatomy, pathology, and surgery of the brain and spinal cord are some of the lecture topics developed and delivered by Clinical Anatomy Associates, Inc.
Image modified from the original (in the public domain) by Sobotta (1945)
- Details
This article is part of the series "A Moment in History" where we honor those who have contributed to the growth of medical knowledge in the areas of anatomy, medicine, surgery, and medical research.

Click for a larger image
Dr. Húmer Hültl (1868 – 1940) Hungarian surgeon, Húmer Hültl was born in 1868 in Felsobanya. Hültl studied in Budapest, earning his medical degree in 1891, and after surgical training he started to work as a surgeon in 1893.
By 1900, Dr. Hültl was the chief surgeon at the St. Stephen’s Hospital and later at the Sr. Rokus Hospital, and during WWI he was a commander of a Hungarian military hospital. Dr. Hültl’s attention to detail, careful asepsis (after Ignaz Semmelweis) and superb surgical technique earned him the moniker “The Paganini of the Knife”. Hültl was the first in his country to introduce the use of face masks, gloves, sterile cotton, and rubber gloves.
Dr. Hültl was very concerned about the consequences of spillage of gastrointestinal contents in the peritoneal cavity during surgery, covering all the walls of the cavity with sterile towels. At that time some surgical instruments had been invented to keep the edges of the intestines together while suturing. In 1907 Dr. Hültl envisioned a mechanical instrument that could place rows of staples transversely in the intestines thus avoiding spillage. With the aid of Victor Fisher, a German mechanical engineer, the first surgical stapler was constructed.
This original instrument was very bulky and heavy, weighing close to 11 pounds, and used a “bicycle-chain” type of mechanism to push a crankshaft that would push the staples into the anvil to form “B” shaped staples. It placed four rows or staggered staples. This device was first used in surgery on May 9th, 1908. A later, lighter variation of the instrument was later created, with a different crankshaft and weighing 8 pounds. Images of these instruments are available here.
Not many of these instruments were sold, but Dr. Hültl had set the stage for the development of the modern surgical stapler. Even today we still use the basic principles of his surgical stapler: “B" shaped staples, staggered rows of staples, and attention to the avoidance of leakage through the staple line. All of this makes Dr. Hültl an integral part of the history of surgical stapling.
Sources:
1. "Húmer Hültl: The Father of the Surgical Stapler" Robicsek, F.& Konstantinov, I. J Med Biogr February 2001 9: 16-19
2. “Current Practice of Surgical Stapling" Ravitch, MM; Steichen, FM, 1991.
Original image courtesy of "Surgical Stapler Museum" at www.surgicalstaplermuseum.com
- Details
The root term [-mur-] has its origin in the Latin word [murus] and means "wall". In medical terminology it is used mostly as [-mural] meaning "pertaining to a wall". It can be used in the following terms:
• Transmural: Through a wall
• Extramural: Outside a wall
• Intramural: Within a wall
Another term meaning "wall" is [parietal] from the Greek word [paries].
- Details
In medical terms a [sign] is an objective, observable, measurable expression of a pathology. To a physician, the combination of a patient's clinical and familial history (anamnesis), combined with the patient's symptoms and signs allows for a proper diagnosis. Some signs are so subtle and specific that they can only be observed and understood by a trained health care professional. Furthermore, some signs are pathognomonic, that is, by their presence they define a pathology. Furthermore
Contrary to symptoms (which are subjective), signs are not only objective, but comparable between individuals of the same species. Therefore we can compare the heart rate bmp (beats per minute) between normal and sick individuals allowing us to chart a range from normal to abnormal. The same is true for most signs such as body temperature, respiratory capacity, breathing rate, weight, height, etc.
Some signs are particular to a pathology, although they may not be pathognomonic. These specific signs are usually eponymic, such as:
• McMurray's sign: A click caused by the meniscus during manipulation of the knee; indicative of meniscal injury.
• Blumberg's sign: Sharp piercing pain on the abrupt release of steady pressure over the site of a suspected abdominal lesion, indicative of peritonitis. When used to diagnose appendicitis over McBurney's point it may be called Aaron's sign.
• Musset's sign: Rhythmical jerking of the head following the heart pulsations in aortic aneurysm and aortic insufficiency.
• Cardarelli's sign: An abnormal pulsation of the trachea that may be found in patients with an aneurysm of the aortic arch that causes left tracheal displacement.
• Caput medusae: A ring of dilated varicose veins radiating from the umbilicus, usually indicative of portal hypertension.
• Papal Benediction Sign: A contraction of the fourth and fifth digits, as in benediction (see image).
There are many more medical signs, this list is only an illustration of the concept
- Details
The medical term [symptom] has many definitions, as shown in this article. A good definition follows: A symptom is that what a patient refers, it is subjective, and cannot be measured or standardized (between patients). Examples of symptoms are thermal sensation ("I feel hot or feverish"), visceral sensations ("I feel a lump on my throat"), etc. In all cases the main characteristic of a symptom is that is subjective and patient-dependent. It is only relevant to a particular patient and cannot be compared from one patient to another.
Symptoms are part of the clinical study or history of a patient that help lead to a diagnosis.
• Merrian-Webster: "subjective evidence of disease or physical disturbance", "something that indicates the existence of something else"
• Memidex: "any sensation or change in bodily function that is experienced by a patient and is associated with a particular disease"
• Pandora World: "Feelings and perceptions reported by a patient indicative or that can be correlated with a disease process"
• Oxford Dictionaries: "A physical or mental feature that is regarded as indicating a condition of disease, particularly such a feature that is apparent to the patient"
Pain is a subjective entity, as it is characteristic to an individual. We all feel and respond to pain differently, as there are people with higher and lower thresholds to pain. Although I understand the need to have some type of standard, I dread the question posed by many..."From one to ten, can you tell me what your pain level is?. If the answer allows the physician or nurse to compare levels of pain within the same patient and see the evolution of a pathology, I am OK with that. But you cannot use that measurement to compare pain levels between patients!
The latest advances test for nerve activity following a noxa, but this just indicates that pain is being detected. Some say that the higher the recording the higher the pain. Possibly; but since pain is subjective we cannot use that measurement to compare pain levels between patients... at least that is my opinion. Dr. Miranda