Medical Terminology Daily (MTD) is a blog sponsored by Clinical Anatomy Associates, Inc. as a service to the medical community. We post anatomical, medical or surgical terms, their meaning and usage, as well as biographical notes on anatomists, surgeons, and researchers through the ages. Be warned that some of the images used depict human anatomical specimens.
You are welcome to submit questions and suggestions using our "Contact Us" form. The information on this blog follows the terms on our "Privacy and Security Statement" and cannot be construed as medical guidance or instructions for treatment.
We have 971 guests online

Jean George Bachmann
(1877 – 1959)
French physician–physiologist whose experimental work in the early twentieth century provided the first clear functional description of a preferential interatrial conduction pathway. This structure, eponymically named “Bachmann’s bundle”, plays a central role in normal atrial activation and in the pathophysiology of interatrial block and atrial arrhythmias.
As a young man, Bachmann served as a merchant sailor, crossing the Atlantic multiple times. He emigrated to the United States in 1902 and earned his medical degree at the top of his class from Jefferson Medical College in Philadelphia in 1907. He stayed at this Medical College as a demonstrator and physiologist. In 1910, he joined Emory University in Atlanta. Between 1917 -1918 he served as a medical officer in the US Army. He retired from Emory in 1947 and continued his private medical practice until his death in 1959.
On the personal side, Bachmann was a man of many talents: a polyglot, he was fluent in German, French, Spanish and English. He was a chef in his own right and occasionally worked as a chef in international hotels. In fact, he paid his tuition at Jefferson Medical College, working both as a chef and as a language tutor.
The intrinsic cardiac conduction system was a major focus of cardiovascular research in the late nineteenth and early twentieth centuries. The atrioventricular (AV) node was discovered and described by Sunao Tawara and Karl Albert Aschoff in 1906, and the sinoatrial node by Arthur Keith and Martin Flack in 1907.
While the connections that distribute the electrical impulse from the AV node to the ventricles were known through the works of Wilhelm His Jr, in 1893 and Jan Evangelista Purkinje in 1839, the mechanism by which electrical impulses spread between the atria remained uncertain.
In 1916 Bachmann published a paper titled “The Inter-Auricular Time Interval” in the American Journal of Physiology. Bachmann measured activation times between the right and left atria and demonstrated that interruption of a distinct anterior interatrial muscular band resulted in delayed left atrial activation. He concluded that this band constituted the principal route for rapid interatrial conduction.
Subsequent anatomical and electrophysiological studies confirmed the importance of the structure described by Bachmann, which came to bear his name. Bachmann’s bundle is now recognized as a key determinant of atrial activation patterns, and its dysfunction is associated with interatrial block, atrial fibrillation, and abnormal P-wave morphology. His work remains foundational in both basic cardiac anatomy and clinical electrophysiology.
Sources and references
1. Bachmann G. “The inter-auricular time interval”. Am J Physiol. 1916;41:309–320.
2. Hurst JW. “Profiles in Cardiology: Jean George Bachmann (1877–1959)”. Clin Cardiol. 1987;10:185–187.
3. Lemery R, Guiraudon G, Veinot JP. “Anatomic description of Bachmann’s bundle and its relation to the atrial septum”. Am J Cardiol. 2003;91:148–152.
4. "Remembering the canonical discoverers of the core components of the mammalian cardiac conduction system: Keith and Flack, Aschoff and Tawara, His, and Purkinje" Icilio Cavero and Henry Holzgrefe Advances in Physiology Education 2022 46:4, 549-579.
5. Knol WG, de Vos CB, Crijns HJGM, et al. “The Bachmann bundle and interatrial conduction” Heart Rhythm. 2019;16:127–133.
6. “Iatrogenic biatrial flutter. The role of the Bachmann’s bundle” Constán E.; García F., Linde, A.. Complejo Hospitalario de Jaén, Jaén. Spain
7. Keith A, Flack M. The form and nature of the muscular connections between the primary divisions of the vertebrate heart. J Anat Physiol 41: 172–189, 1907.
"Clinical Anatomy Associates, Inc., and the contributors of "Medical Terminology Daily" wish to thank all individuals who donate their bodies and tissues for the advancement of education and research”.
Click here for more information
- Details
The medical term [tenesmus] originates from the Greek [τεινεσμός], itself derivation from [τέντωμα] meaning "stretch", "distend", or to "strain". It refers to a symptom where the patient refers a constant urge to evacuate, with no or ineffective results. There are two types of tenesmus: rectal tenesmus and vesical tenesmus.
Because of the constant straining, tenesmus patients can have pain and cramping. Tenesmus can be one of the symptoms associated with the distal empty segment of colon or rectum found in a temporary or permanent diverting colostomy.
Note: The links to Google Translate in these articles include an icon that will allow you to hear the Greek or Latin pronunciation of the word.
- Details
This article is part of the series "A Moment in History" where we honor those who have contributed to the growth of medical knowledge in the areas of anatomy, medicine, surgery, and medical research.

Mark M. Ravitch, MD
Mark M. Ravitch M.D.(1910-1989) American surgeon, historian, teacher, author, innovator, and visionary, Mark Mitchell Ravitch was born in 1910 in New York City. His parents were Russian immigrants, allowing to be fluent in Russian, which opened the doors to one of his many contributions to medicine and surgery: modern surgical stapling.
In 1934, Dr. Ravitch obtained his MD from Johns Hopkins, continuing in the same institution as a surgical intern, and later as a pediatrics resident, where he worked with Dr. Alfred Blalock, eventually becoming a professor of Surgery at Johns Hopkins, moving later to the Baltimore City Hospital. From 1943 to 1946 Dr. Ravitch was a surgeon in the Army.
He moved to the University of Chicago where from 1966 to 1969 he was professor of pediatric surgery and chief of pediatric surgery. His later and last move was to Pittsburgh, where he was professor of surgery at the University of Pittsburgh, and surgeon-in-chief at the Montefiore Hospital in Pittsburgh.
Dr. Ravitch is known for many important contributions to surgery, especially pediatric surgery, where he pioneered a procedure (the eponymic Ravitch procedure) to repair pectum excavatum in children, as well as research and develop a of nonoperative procedure to reduce intussuception using hydrostatic pressure reduction with barium enema. For this and many contributions he is known as one of the founding fathers of pediatric surgery.
A prolific writer and visionary, Dr. Ravitch authored 453 papers, 101 book chapters, 22 books, and served as editor of nearly 20 medical journals. In some of his writings he presented his vision for the development of surgery, even to the point of predicting heart transplantation surgery. Dr. Ravitch also was a surgical historian, with a wonderful library that was donated to the University of Pittsburgh upon his death.
In the medical industry Dr. Mark Ravitch is probably best know for bringing to the USA from the then USSR, the technology of surgical stapling. In 1958, while visiting Kiev, Dr. Ravitch and three other American physicians were shown the use in surgery of a bronchial surgical stapler developed in the USSR. They were able to procure one of these devices and bring it back to the USA. An American entrepreneur, Leon Hirsch, obtained the patents for these devices, founded the United States Surgical Corporation (now the Covidien Surgical Devices Division) and continued the development of the reusable and later the disposable surgical staplers. During the research Dr. Ravitch was joined by Dr. Felicien Steichen (1926 - 2011). Both Drs. Ravitch and Steichen were instrumental in the research and development of these modern surgical devices, making them part of the history of surgical stapling. Their work set the stage for the development of surgical stapling in minimally invasive procedures, so common today.
Dr. Ravitch died in 1989, still teaching students from his own hospital bed. His son Dr. Michael M. Ravitch (1943-2004) followed in his steps in medical education as an educational psychologist at Northwestern University's Feinberg School of Medicine.
Personal notes: I regret not having had the opportunity to meet Dr. Ravitch. In 2006 I spent several hours talking with Dr. Felicien Steichen about his trip to the USSR with Dr. Ravitch and the research and development that happened afterwards. When concluding my visit, Dr. Steichen presented me with a signed copy of his and Dr. Ravitch's book that reads:"Mark Ravitch would have enthusiastically applauded your efforts to teach the science of Anatomy that is the basis of the Art of Surgery". With the loss of both Drs. Ravitch and Steichen a wonderful chapter of the history of surgical stapling has closed.
A few years ago I was contacted by the Ravitch family. Knowing of my interest in Medical History, they donated a series of books signed by Dr. Ravitch. Recently the family also donated the personally typed diary of his trip tp Russia in 1958. They will be well cared and hopefully I will be able to have them printed as a book in the future. Dr. Miranda.
Sources:
1. "Naissance des sutures mecaniques modernes en chirurgie: petites et grandes histoires, en hommage a Mark Ravitch" Steichen,FM Chirurgie 1998,123 (6), 616.
2. "The Peaks of Excitement" Ann Surg 192: (1980) 3, 282 - 287
3. "A Century of Surgery, 1880-1980" Ravitch, Mark M.. Philadelphia
4. "Current Practice of Surgical Stapling" Ravitch, W & Steichen, F. 1991 Lea & Febiger USA
5. "Mark Ravitch (1910 - 1989) Editors, "Current Problems in Surgery" 1989
6. "All heart - Mark Ravitch" O'Donell B. J Ped Surg 25:1 (1990) 184
7. "Mark M. Ravitch: Historian and Innovator" Fingerete, AL, et al. J Surg Ed (2011) 155-158
8. "Reduction of intussusception by barium enema : A clinical and experimental study" Ravitch MM, McCune RM.Ann Surg. 1948;128:904-91
9. "The Surgical Curmudgeon" Pittmed, Spring 2013. 18-23
- Details
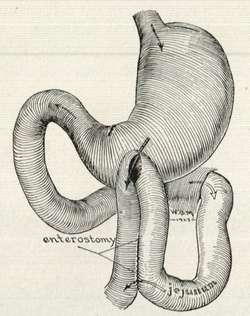
This is a Greek compound word. [ana-] meaning "through or complete", the root term [-stom-] from [stoma], meaning "mouth or opening" and the suffix [-osis] meaning "condition". Usually [-osis] refers to a disease, but in this case it refers to an action or process. The plural form for [anastomosis] is [anastomoses].
The word [anastomosis] then refers to the "process or action of creating a complete opening". In reality an anastomosis is the process of creating a permanent opening between two structures which allows for drainage or flow from one structure into the other. The suffix [-ostomy], being the term for "drainage" is the best suffix to describe an anastomosis. An anastomosis can be the result of a surgical procedure or found as a natural occurrence, such as the anastomoses found in the arterial circle of Willis or an abnormal fistula.
The accompanying image shows an early 1900's depiction of an anterior gastrojejunostomy. The term [gastrojejunostomy] is then the "creation of a drainage opening (a common mouth or opening) between the stomach and the jejunum, the second portion of the small intestine.
It is our belief and core competency, that surgical medical device sales representatives and managers should be completely familiar with this medical term, as well as the many types of anastomoses that can be performed surgically. To this end, we have developed a video on the History of Surgical Stapling. At the end of a video you can see a demonstration of the use of these devices to create an anastomosis
- Details
The [falx cerebri] is a falciform or sickle-shaped median extension of the dura mater found within the cranial cavity. It is narrow anteriorly, where it attaches to the crista galli of the ethmoid bone and widens posteriorly, where it ends when it meets another dura mater extension, the tentorium cerebelli.
The falx cerebri is found in the interhemispheric fissure of the brain, separating both cerebral hemispheres. Its inferior free edge is closely related to the corpus callosum.
Reduplications of the dura mater forming the falx cerebri creates venous channels known as "sinuses". The superior border of the falx cerebri, where it meets the dura mater covering the brain forms the [superior longitudinal sinus]. The inferior free border of the falx cerebri forms the [inferior longitudinal sinus], and at the junction of the falx cerebri with the tentorium cerebelli we find the [longitudinal sinus].
The Latin word [falx] (plural [falcis]) means "scythe" or "sickle".
Original image, public domain, courtesy of Wikipedia
- Details
UPDATED: The root for this word comes from the Latin [falx] (plural [falcis]) meaning "scythe" or "sickle". [Falciform] means "shaped like a sickle or a scythe". The term [falx cerebri] is used to name the sickle-shaped median extension of the dura mater that separates both cerebral hemispheres.
There are several falciform structures in the human body, such as the falciform ligament of the lung, more commonly known as the pulmonary ligament, and the falciform margin of the saphenous opening, the edge of a foramen in the femoral fascia to allow passage of the greater saphenous vein.
The most commonly known use of the term is the "falciform ligament of the liver", a sickle-shaped extension of peritoneum that connects the liver capsule (Glisson's) to the peritoneal covering of the abdominal wall (parietal peritoneum). At the free edge of the falciform ligament and covered by peritoneum run the round ligament of the liver (an embryological remnant of fetal circulation) and the paraumbilical veins.
- Details
The medical term [vaccine] originates from the Latin term [vacca] meaning "cow". The Latin adjectival form is [vaccinus].
The word originated from the work of Edward Jenner (1749 - 1823) who, based in observation, developed an injection of cowpox virus and injected them into patients, rendering them inmune to smallpox. This extraordinary discovery was the basis for the Balmis Expedition to the New World.
Since the cowpox virus was extracted initally from cows (Lat:vacca), and later from human cowpox sores, and Latin was at the time the preferred language of medical communication, the word "vaccina" was created. Evolution of the word led to the English [vaccine] and Spanish [vacuna]