Medical Terminology Daily (MTD) is a blog sponsored by Clinical Anatomy Associates, Inc. as a service to the medical community. We post anatomical, medical or surgical terms, their meaning and usage, as well as biographical notes on anatomists, surgeons, and researchers through the ages. Be warned that some of the images used depict human anatomical specimens.
You are welcome to submit questions and suggestions using our "Contact Us" form. The information on this blog follows the terms on our "Privacy and Security Statement" and cannot be construed as medical guidance or instructions for treatment.
We have 769 guests and no members online

Jean George Bachmann
(1877 – 1959)
French physician–physiologist whose experimental work in the early twentieth century provided the first clear functional description of a preferential interatrial conduction pathway. This structure, eponymically named “Bachmann’s bundle”, plays a central role in normal atrial activation and in the pathophysiology of interatrial block and atrial arrhythmias.
As a young man, Bachmann served as a merchant sailor, crossing the Atlantic multiple times. He emigrated to the United States in 1902 and earned his medical degree at the top of his class from Jefferson Medical College in Philadelphia in 1907. He stayed at this Medical College as a demonstrator and physiologist. In 1910, he joined Emory University in Atlanta. Between 1917 -1918 he served as a medical officer in the US Army. He retired from Emory in 1947 and continued his private medical practice until his death in 1959.
On the personal side, Bachmann was a man of many talents: a polyglot, he was fluent in German, French, Spanish and English. He was a chef in his own right and occasionally worked as a chef in international hotels. In fact, he paid his tuition at Jefferson Medical College, working both as a chef and as a language tutor.
The intrinsic cardiac conduction system was a major focus of cardiovascular research in the late nineteenth and early twentieth centuries. The atrioventricular (AV) node was discovered and described by Sunao Tawara and Karl Albert Aschoff in 1906, and the sinoatrial node by Arthur Keith and Martin Flack in 1907.
While the connections that distribute the electrical impulse from the AV node to the ventricles were known through the works of Wilhelm His Jr, in 1893 and Jan Evangelista Purkinje in 1839, the mechanism by which electrical impulses spread between the atria remained uncertain.
In 1916 Bachmann published a paper titled “The Inter-Auricular Time Interval” in the American Journal of Physiology. Bachmann measured activation times between the right and left atria and demonstrated that interruption of a distinct anterior interatrial muscular band resulted in delayed left atrial activation. He concluded that this band constituted the principal route for rapid interatrial conduction.
Subsequent anatomical and electrophysiological studies confirmed the importance of the structure described by Bachmann, which came to bear his name. Bachmann’s bundle is now recognized as a key determinant of atrial activation patterns, and its dysfunction is associated with interatrial block, atrial fibrillation, and abnormal P-wave morphology. His work remains foundational in both basic cardiac anatomy and clinical electrophysiology.
Sources and references
1. Bachmann G. “The inter-auricular time interval”. Am J Physiol. 1916;41:309–320.
2. Hurst JW. “Profiles in Cardiology: Jean George Bachmann (1877–1959)”. Clin Cardiol. 1987;10:185–187.
3. Lemery R, Guiraudon G, Veinot JP. “Anatomic description of Bachmann’s bundle and its relation to the atrial septum”. Am J Cardiol. 2003;91:148–152.
4. "Remembering the canonical discoverers of the core components of the mammalian cardiac conduction system: Keith and Flack, Aschoff and Tawara, His, and Purkinje" Icilio Cavero and Henry Holzgrefe Advances in Physiology Education 2022 46:4, 549-579.
5. Knol WG, de Vos CB, Crijns HJGM, et al. “The Bachmann bundle and interatrial conduction” Heart Rhythm. 2019;16:127–133.
6. “Iatrogenic biatrial flutter. The role of the Bachmann’s bundle” Constán E.; García F., Linde, A.. Complejo Hospitalario de Jaén, Jaén. Spain
7. Keith A, Flack M. The form and nature of the muscular connections between the primary divisions of the vertebrate heart. J Anat Physiol 41: 172–189, 1907.
"Clinical Anatomy Associates, Inc., and the contributors of "Medical Terminology Daily" wish to thank all individuals who donate their bodies and tissues for the advancement of education and research”.
Click here for more information
- Details
This article is part of the series "A Moment in History" where we honor those who have contributed to the growth of medical knowledge in the areas of anatomy, medicine, surgery, and medical research.

Jan Evangelista Purkinje
Jan Evangelista Purkinje (1787 - 1869). Known by his German name Purkinje, or his Czech name, Purkyn?, as well as his church-given name Salverius. Purkinje was born in the city of Libochovice, Bohemia, (now Czechoslovakia). He started his early studies in the church with Piarist monks. He took the name of Brother Salverius and served as a teacher in the Piarist schools. He dedicated himself to the study of natural sciences. Purkinje left the monastery before taking his final vows. Purkinje continued his studies and graduated in medicine in Prague. Even as a student Purkinje started research on the physics of sound and the physiology of vision, which he continued after his graduation. Purkinje was one of the first to understand the vision of motion, thus creating the first animated cartoons!
In 1823 Purkinje was appointed Professor of Physiology at the University of Wroclaw (Breslau), later taking the same chair in Prague. Besides being one of the first to propose experimental physiology as basis for research, Purkinje was one of the first to use the microscope to study the cells of the body, proposing the "cell theory", and introducing the word "protoplasm".
He made a number of discoveries, and his name is eponymically tied to many structures and processes, such as:
- Purkinje's cell of the cerebellum: Piriform cells found in Purkinje's layer
- Purkinje's fibers of the heart: These are not "fibers" as the name implies, but fast-conducting myocardial cells found as the most distal components of the conduction system of the heart
- Purkinje's law of vertigo: An observation that the apparent motion perceived when stopping the head after rotation changes from horizontal to vertical if the head is inclined laterally. This is important to pilots, as they are trained to understand that in conditions without external reference, moving the head down or laterally can induce uncontrollable vertigo.
Sources:
1. "Purkinje JE (1845) Mikroskopisch-neurologische Beobachturgen" Arch Anat Physiol Wiss Med II/III:281-295
2. "Jan Evangelista Purkinje (1787-1869)" J Neurol Neurosurg Psychiatry. 1994 July; 57(7): 777
3. "Jan Evangelista Purkinje (1787-1869)" Davies, MK; Hollman A. Heart (1996) 76(4): 311
- Details
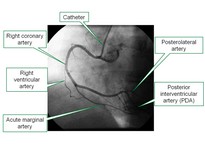
The root term [-angi-] has Greek origins and means "vessel", as in a "container". The suffix [(o)gram] means "examination of", or a "record". An angiogram is the examination of a vessels using some type of viewing or recording device.
In an angiogram the physician will inject radiopaque contrast to make the vessels discernible in an X-ray machine.
The accompanying image is an angiogram of the right coronary artery. It can also be called a "coronariogram".
The image shows the right coronary artery and three key branches: the acute marginal artery, the posterolateral artery, and the posterior interventricular artery (PDA).
- Details
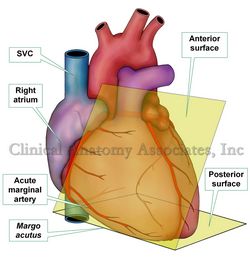
The "acute margin" refers to the anteroinferior border of the heart. It is also known by its Latin name [margo acutus].
The name of this border or margin of the heart is quite descriptive. If you observe the angle formed between the anterior or sternocostal surface of the heart with the posterior or diaphragmatic surface of the heart, you can see that the angle between these two surfaces is less than 90 degrees, therefore an "acute" angle. The corresponding border between these two surfaces has to be called the "acute margin"!
In relation to the acute margin of the heart there is usually found one of the longest branches of the right coronary artery. This artery that runs alongside the acute margin, is the "acute marginal artery", In an angiogram, this artery clearly depicts the anteroinferior border of the heart.
Here is a link to the article on the "obtuse margin" of the heart.
- Details
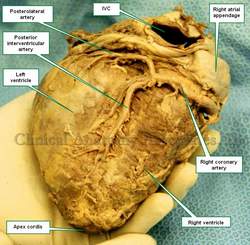
The posterolateral artery, also known as the "retroventricular artery" is one of the two terminal branches of the right coronary artery. The other terminal branch is the posterior interventricular artery or PDA. This artery presents with many variations, from being absent to extremely long arteries with extensive branching that take some of the territory of the circumflex artery. The posterolateral artery extends from the crux cordis to the left side of the heart in the atrioventricular sulcus.
The AV node artery, which provides blood supply to the atrioventricular node (a component of the conduction system of the heart) may arise from the posterolateral artery instead of arising from the right coronary artery or the posterior interventricular artery.
When present, the posterolateral artery provides some posterior left ventricular branches and maybe some posterior left atrial branches. See the accompanying image, you may click on the image for more information. The image depicts a posterolateral artery slightly longer than usual.
Image property of: CAA, Inc. Photographer: E. Klein
- Details
This article is part of the series "A Moment in History" where we honor those who have contributed to the growth of medical knowledge in the areas of anatomy, medicine, surgery, and medical research.
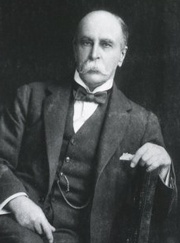
Sir William Osler
Sir William Osler (1849-1919). William Osler was born in Bond Head, Canada, in what today is known as Ontario, of English parents. He started his college studies to become a minister, but realizing his true vocation was in medicine, he entered the Toronto School of Medicine, earning his medical degree in 1872.
Osler completed postgraduate studies in Europe, returning as a Professor at the McGill University. In 1884 he moved to Philadelphia to the University of Pennsylvania. In 1889 he left to become Physician-in-Chief and one of the founders of the newly-built John Hopkins hospital. His contributions to this new hospital and the American medical education are innumerable. Dr. Osler initiated the residency programs used today, as well as the programs of third and fourth year medical students in bedside patient rounds.
A prolific writer, Dr. Osler penned over 1,500 articles, monographs, and books, some of which are famous. His “Principles and Practice of Medicine” was published for a record 17 editions and 76 years (1892 -1968)! One of his most famous addresses is “Aequanimitas”, which he delivered when leaving the University of Pennsylvania.
In 1905 Dr. Osler accepted the position of Royal Chair of Medicine at Oxford, in England, and in 1911 he was awarded the title of “Sir William Osler”.
Personal Note: In June 1999, I had the opportunity to visit the collection of the John Martin Rare Book Room at the University of Iowa Medical School. I was allowed to read and handle original copies of the Fabrica and the Epitome by Vesalius as well as other original and rare medical books, including De Muto Cordis, by William Harvey. The books I had the opportunity to review were placed on an antique desk that belonged to Sir William Osler. A moment that has stayed with me, as it was the confluence of great individuals: Andreas Vesalius, the anatomist; William Harvey, the physiologist, and Sir William Osler, the medical educator. Dr. Miranda
Sources:
“Sir William Osler, M.D., C.M.” Sarik, J. Yeo, Ch.Pinckney J. The American Surgeon78.4 (2012): 385-7.
“Sir William Osler and gastroenterology” Chaun H. Can J Gastroenterol (2010) 24:10 615-618
“Sir William Osler (1849-1919)” Haas, LF J Neurol Neurosurg Psychiatry 1999 67: 137
“Sir William Osler (1849-1919)”Christian, HA Proc Amer Acad Arts Sci (1922) 496-499