Medical Terminology Daily (MTD) is a blog sponsored by Clinical Anatomy Associates, Inc. as a service to the medical community. We post anatomical, medical or surgical terms, their meaning and usage, as well as biographical notes on anatomists, surgeons, and researchers through the ages. Be warned that some of the images used depict human anatomical specimens.
You are welcome to submit questions and suggestions using our "Contact Us" form. The information on this blog follows the terms on our "Privacy and Security Statement" and cannot be construed as medical guidance or instructions for treatment.
We have 236 guests and no members online

Jean George Bachmann
(1877 – 1959)
French physician–physiologist whose experimental work in the early twentieth century provided the first clear functional description of a preferential interatrial conduction pathway. This structure, eponymically named “Bachmann’s bundle”, plays a central role in normal atrial activation and in the pathophysiology of interatrial block and atrial arrhythmias.
As a young man, Bachmann served as a merchant sailor, crossing the Atlantic multiple times. He emigrated to the United States in 1902 and earned his medical degree at the top of his class from Jefferson Medical College in Philadelphia in 1907. He stayed at this Medical College as a demonstrator and physiologist. In 1910, he joined Emory University in Atlanta. Between 1917 -1918 he served as a medical officer in the US Army. He retired from Emory in 1947 and continued his private medical practice until his death in 1959.
On the personal side, Bachmann was a man of many talents: a polyglot, he was fluent in German, French, Spanish and English. He was a chef in his own right and occasionally worked as a chef in international hotels. In fact, he paid his tuition at Jefferson Medical College, working both as a chef and as a language tutor.
The intrinsic cardiac conduction system was a major focus of cardiovascular research in the late nineteenth and early twentieth centuries. The atrioventricular (AV) node was discovered and described by Sunao Tawara and Karl Albert Aschoff in 1906, and the sinoatrial node by Arthur Keith and Martin Flack in 1907.
While the connections that distribute the electrical impulse from the AV node to the ventricles were known through the works of Wilhelm His Jr, in 1893 and Jan Evangelista Purkinje in 1839, the mechanism by which electrical impulses spread between the atria remained uncertain.
In 1916 Bachmann published a paper titled “The Inter-Auricular Time Interval” in the American Journal of Physiology. Bachmann measured activation times between the right and left atria and demonstrated that interruption of a distinct anterior interatrial muscular band resulted in delayed left atrial activation. He concluded that this band constituted the principal route for rapid interatrial conduction.
Subsequent anatomical and electrophysiological studies confirmed the importance of the structure described by Bachmann, which came to bear his name. Bachmann’s bundle is now recognized as a key determinant of atrial activation patterns, and its dysfunction is associated with interatrial block, atrial fibrillation, and abnormal P-wave morphology. His work remains foundational in both basic cardiac anatomy and clinical electrophysiology.
Sources and references
1. Bachmann G. “The inter-auricular time interval”. Am J Physiol. 1916;41:309–320.
2. Hurst JW. “Profiles in Cardiology: Jean George Bachmann (1877–1959)”. Clin Cardiol. 1987;10:185–187.
3. Lemery R, Guiraudon G, Veinot JP. “Anatomic description of Bachmann’s bundle and its relation to the atrial septum”. Am J Cardiol. 2003;91:148–152.
4. "Remembering the canonical discoverers of the core components of the mammalian cardiac conduction system: Keith and Flack, Aschoff and Tawara, His, and Purkinje" Icilio Cavero and Henry Holzgrefe Advances in Physiology Education 2022 46:4, 549-579.
5. Knol WG, de Vos CB, Crijns HJGM, et al. “The Bachmann bundle and interatrial conduction” Heart Rhythm. 2019;16:127–133.
6. “Iatrogenic biatrial flutter. The role of the Bachmann’s bundle” Constán E.; García F., Linde, A.. Complejo Hospitalario de Jaén, Jaén. Spain
7. Keith A, Flack M. The form and nature of the muscular connections between the primary divisions of the vertebrate heart. J Anat Physiol 41: 172–189, 1907.
"Clinical Anatomy Associates, Inc., and the contributors of "Medical Terminology Daily" wish to thank all individuals who donate their bodies and tissues for the advancement of education and research”.
Click here for more information
- Details

Click for a larger image
From the Greek [spondylos] meaning "vertebra", its combining form is [spondylo-]. Use of this term include:
- Spondylitis: Inflammation of a vertebra.
- Spondylosis: The suffix [-osis] means "condition", but with the connotation of "many". The term means "many vertebrae", but it refers to excessive abnormal growth of portions of the vertebral body, usually forming "bone spurs", also referred to as "spondylophytes"
- Spondylolysis: From the Greek [lysis], meaning "loosening", the term is used to mean "destruction" or "breaking of". Spondylolysis refers to the breakage, destruction, or loosening of part of a vertebra.
- Spondylolisthesis: From the Greek term [olisthos] meaning "slippery". A "slippery vertebra", referring to the anterior (or posterior) displacement of a vertebra over another one.
Image property of: CAA.Inc. Photographer: David M. Klein
- Details
This article is part of the series "A Moment in History" where we honor those who have contributed to the growth of medical knowledge in the areas of anatomy, medicine, surgery, and medical research.
Peter Paul Broca (1824- 1880). Surgeon and anthropologist, Peter Paul Broca was born in Sainte-Foy-la-Grande in France. His earlier studies were in mathematics, but graduated in medicine, becoming a professor of clinical surgery. He became interested in anthropology and applied his mathematical expertise to the measurement and interpretation of his findings in comparative anatomy.
Broca was the founder of the first Anthropological Society of Paris, and used this venue to deliver most of his work. A prolific writer, Broca published over 500 scientific papers and several books. At one of the meetings of the society the discussion was directed to brain areas and speech. Broca had a patient with a condition that he referred to as aphemia (later known as aphasia); this patient died a few days later and upon autopsy, Broca was able to see a distinct cavity in the left lateral frontal lobe. Upon finding the same situation in another patient, he was able to describe the area of the brain responsible for speech, known today as "Broca's area" in the third left frontal brain convolution. Broca is responsible for naming many of the craniometric points in the human skull such as bregma, dacryon, inion, lambda, metopion, etc.
Broca was part of the discovery and study of the Neanderthal man. He remained the secretary of the Anthropological Society of Paris until his death in 1880.
Original image in the public domain, courtesy of National Institutes of Health.
- Details
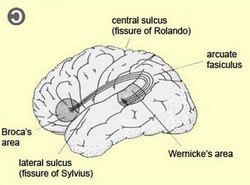
The term [aphasia] has Greek origins and means "without speech". This pathology was first described by Paul Broca who called it "aphemia".
Aphasia is a total and complete loss of speech. Lesser presentations of this condition should be called [dysphasias) from the prefix [dys-] meaning "abnormal", and [phasia], meaning "speech".
Aphasia is the lack of spoken speech due to cerebral cortex damage in the dominant brain hemisphere, usually the left side in right-handed individuals. There are two main areas of the brain involved in speech: Broca's and Wernicke's. Broca's area is responsible for speech expression (the spoken and written word). Damage to this area causes expressive or motor aphasia (or dysphasia).
Wernicke's area is responsible for the comprehension of speech, the understanding of language. Damage to this area causes receptive or sensory aphasia (or dysphasia). Broca's and Wernicke's areas are connected by an intrahemispheric tract known as the arcuate fasciculus (see image).
pathologies are:
- Agraphia / dysgraphia: Incapacity / difficulty in writing
- Anomia / dysnomia: Incapacity / difficulty in naming objects
- Aphrasia / dysphrasia: Incapacity / difficulty forming phrases or sentences. The patient can communicate with single words, but cannot form sentences.
Image under copyleft agreement courtesy of The Brain from Top to Bottom
- Details
The scaphoid is one of the proximal carpal bones that form the wrist. The name arises from the Greek [scaphe], meaning "boat"; and [-oid], meaning "similar to". The scaphoid bone roughly resembles a rowboat. It is also known as the navicular bone (from the Latin [navis] meaning "boat"), and os naviculare manus.
Proximally, the scaphoid bone articulates with the radius. Distally, the scaphoid articulates with the trapezium and trapezoid bones. On its medial aspect, the scaphoid bone has two articular surfaces for the lunate and the hamate bones. The scaphoid bone also has very strong ligamentous connections with the lunate bone by way of the scapholunate interosseous ligament
The accompanying image shows the anterior (volar) surface of the wrist.
Image modified from the original: "3D Human Anatomy: Regional Edition DVD-ROM." Courtesy of Primal Pictures
- Details
The terms [medial] and [lateral] are opposing anatomical relationship terms that indicate the location of a structure or structures in relation to the midline or median plane. The accompanying image depicts the median plane.
The term "midline" is a bit of a misnomer, as this is a plane and not a line, although if you look at the median plane from the anterior or posterior aspect of an individual in the anatomical position, you would have a line, ergo, midline! Look at this article on the anatomical position to see an explanation and image of this concept.
The term [medial] means "closer to the midline". An example of the use of this term is: "the head of the clavicle is medial to the shoulder joint", that is, the head of the clavicle is closer to the midline than the shoulder joint.
The term [lateral] means "further from the midline". An example of the use of this term is: "the wrist joint is lateral to the elbow joint", that is, the wrist joint is further away from the midline than the elbow joint.
Click on the image for a visual explanation of the concepts of "medial" and "lateral".
Images property of: CAA.Inc. Artist: Victoria G. Ratcliffe
- Details
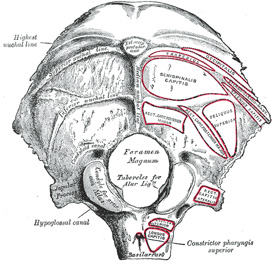
External view of the occipital bone
The term [inion] is Greek [ινιον] and originally referred to the posterior aspect of the neck or occiput and its musculature and strength, as mentioned in the Iliad.
The term fell in disuse for hundreds of years, until it was resurrected by Peter Paul Broca (1824-1880) as a craniometric point. The inion is the midline protuberance in the posteroinferior aspect of the external surface of the occipital bone. Today, in most anatomy texts the inion is referred to as the "external occipital protuberance"
The inion is found at the intersection of three bony lines that are easily palpable, the bilaterally situated superior nuchal line, and the median nuchal line. It is labeled "Ext. occip. protuberance" (see accompanying image). There is a corresponding internal occipital protuberance in the internal aspect of the occipital bone.
Sources:
1. "The Origin of Medical Terms" Skinner, HA 1970 Hafner Publishing Co.
2. "Medical Meanings - A Glossary of Word Origins" Haubrich, WD. ACP Philadelphia
3 "Tratado de Anatomia Humana" Testut et Latarjet 8 Ed. 1931 Salvat Editores, Spain
4. "Anatomy of the Human Body" Henry Gray 1918. Philadelphia: Lea & Febiger
Image modified by CAA, Inc. Original image by Henry Vandyke Carter, MD., courtesy of bartleby.com