Medical Terminology Daily (MTD) is a blog sponsored by Clinical Anatomy Associates, Inc. as a service to the medical community. We post anatomical, medical or surgical terms, their meaning and usage, as well as biographical notes on anatomists, surgeons, and researchers through the ages. Be warned that some of the images used depict human anatomical specimens.
You are welcome to submit questions and suggestions using our "Contact Us" form. The information on this blog follows the terms on our "Privacy and Security Statement" and cannot be construed as medical guidance or instructions for treatment.
We have 877 guests online

Jean George Bachmann
(1877 – 1959)
French physician–physiologist whose experimental work in the early twentieth century provided the first clear functional description of a preferential interatrial conduction pathway. This structure, eponymically named “Bachmann’s bundle”, plays a central role in normal atrial activation and in the pathophysiology of interatrial block and atrial arrhythmias.
As a young man, Bachmann served as a merchant sailor, crossing the Atlantic multiple times. He emigrated to the United States in 1902 and earned his medical degree at the top of his class from Jefferson Medical College in Philadelphia in 1907. He stayed at this Medical College as a demonstrator and physiologist. In 1910, he joined Emory University in Atlanta. Between 1917 -1918 he served as a medical officer in the US Army. He retired from Emory in 1947 and continued his private medical practice until his death in 1959.
On the personal side, Bachmann was a man of many talents: a polyglot, he was fluent in German, French, Spanish and English. He was a chef in his own right and occasionally worked as a chef in international hotels. In fact, he paid his tuition at Jefferson Medical College, working both as a chef and as a language tutor.
The intrinsic cardiac conduction system was a major focus of cardiovascular research in the late nineteenth and early twentieth centuries. The atrioventricular (AV) node was discovered and described by Sunao Tawara and Karl Albert Aschoff in 1906, and the sinoatrial node by Arthur Keith and Martin Flack in 1907.
While the connections that distribute the electrical impulse from the AV node to the ventricles were known through the works of Wilhelm His Jr, in 1893 and Jan Evangelista Purkinje in 1839, the mechanism by which electrical impulses spread between the atria remained uncertain.
In 1916 Bachmann published a paper titled “The Inter-Auricular Time Interval” in the American Journal of Physiology. Bachmann measured activation times between the right and left atria and demonstrated that interruption of a distinct anterior interatrial muscular band resulted in delayed left atrial activation. He concluded that this band constituted the principal route for rapid interatrial conduction.
Subsequent anatomical and electrophysiological studies confirmed the importance of the structure described by Bachmann, which came to bear his name. Bachmann’s bundle is now recognized as a key determinant of atrial activation patterns, and its dysfunction is associated with interatrial block, atrial fibrillation, and abnormal P-wave morphology. His work remains foundational in both basic cardiac anatomy and clinical electrophysiology.
Sources and references
1. Bachmann G. “The inter-auricular time interval”. Am J Physiol. 1916;41:309–320.
2. Hurst JW. “Profiles in Cardiology: Jean George Bachmann (1877–1959)”. Clin Cardiol. 1987;10:185–187.
3. Lemery R, Guiraudon G, Veinot JP. “Anatomic description of Bachmann’s bundle and its relation to the atrial septum”. Am J Cardiol. 2003;91:148–152.
4. "Remembering the canonical discoverers of the core components of the mammalian cardiac conduction system: Keith and Flack, Aschoff and Tawara, His, and Purkinje" Icilio Cavero and Henry Holzgrefe Advances in Physiology Education 2022 46:4, 549-579.
5. Knol WG, de Vos CB, Crijns HJGM, et al. “The Bachmann bundle and interatrial conduction” Heart Rhythm. 2019;16:127–133.
6. “Iatrogenic biatrial flutter. The role of the Bachmann’s bundle” Constán E.; García F., Linde, A.. Complejo Hospitalario de Jaén, Jaén. Spain
7. Keith A, Flack M. The form and nature of the muscular connections between the primary divisions of the vertebrate heart. J Anat Physiol 41: 172–189, 1907.
"Clinical Anatomy Associates, Inc., and the contributors of "Medical Terminology Daily" wish to thank all individuals who donate their bodies and tissues for the advancement of education and research”.
Click here for more information
- Details
This article is part of the series "A Moment in History" where we honor those who have contributed to the growth of medical knowledge in the areas of anatomy, medicine, surgery, and medical research.
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua.
Henry Vandyke Carter, MD (1831 – 1897). English physician, surgeon, medical artist, and a pioneer in leprosy and mycetoma studies. HV Carter was born in Yorkshire in 1831. He was the son of Henry Barlow Carter, a well-known artist and it is possible that he honed his natural talents with his father. His mother picked his middle name after a famous painter, Anthony Van Dyck. This is probably why his name is sometimes shown as Henry Van Dyke Carter, although the most common presentation of his middle name is Vandyke.
Having problems to finance his medical studies, HV Carter trained as an apothecary and later as an anatomical demonstrator at St. George’s Hospital in London, where he met Henry Gray (1872-1861), who was at the time the anatomical lecturer. Having seen the quality of HV Carter’s drawings, Henry Gray teamed with him to produce one of the most popular and longer-lived anatomy books in history: “Gray’s Anatomy”, which was first published in late 1857. The book itself, about which many papers have been written, was immediately accepted and praised because of the clarity of the text as well as the incredible drawings of Henry Vandyke Carter.
While working on the book’s drawings, HV Carter continued his studies and received his MD in 1856.
In spite of initially being offered a co-authorship of the book, Dr. Carter was relegated to the position of illustrator by Henry Gray and never saw the royalties that the book could have generated for him. For all his work and dedication, Dr. Carter only received a one-time payment of 150 pounds. Dr. Carter never worked again with Gray, who died of smallpox only a few years later.
Frustrated, Dr. Carter took the exams for the India Medical Service. In 1858 he joined as an Assistant Surgeon and later became a professor of anatomy and physiology. Even later he served as a Civil Surgeon. During his tenure with the India Medical Service he attained the ranks of Surgeon, Surgeon-Major, Surgeon-Lieutenant-Colonel, and Brigade-Surgeon.
Dr. Carter dedicated the rest of his life to the study of leprosy, and other ailments typical of India at that time. He held several important offices, including that of Dean of the Medical School of the University of Bombay. In 1890, after his retirement, he was appointed Honorary Physician to the Queen.
Dr. Henry Vandyke Carter died of tuberculosis in 1897.
Personal note: Had history been different, this famous book would have been called “Gray and Carter’s Anatomy” and Dr. Carter never gone to India. His legacy is still seen in the images of the thousands of copies of “Gray’s Anatomy” throughout the world and the many reproductions of his work available on the Internet. We are proud to use some of his images in this blog. The image accompanying this article is a self-portrait of Dr. Carter. Click on the image for a larger depiction. Dr. Miranda
Sources:
1. “Obituary: Henry Vandyke Carter” Br Med J (1897);1:1256-7
2. “The Anatomist: A True Story of ‘Gray’s Anatomy” Hayes W. (2007) USA: Ballantine
3. “A Glimpse of Our Past: Henry Gray’s Anatomy” Pearce, JMS. J Clin Anat (2009) 22:291–295
4. “Henry Gray and Henry Vandyke Carter: Creators of a famous textbook” Roberts S. J Med Biogr (2000) 8:206–212.
5. “Henry Vandyke Carter and his meritorious works in India” Tappa, DM et al. Indian J Dermatol Venereol Leprol (2011) 77:101-3
- Details
This article is part of the series "A Moment in History" where we honor those who have contributed to the growth of medical knowledge in the areas of anatomy, medicine, surgery, and medical research.

Alexander Monro Secundus
Alexander Monro Secundus (1733- 1817). Scottish physician and anatomist, born in Edinburgh. Alexander Monro Secundus (the second), studied anatomy with his father Alexander Monro Primus (the first). He received his doctorate in medicine at 22 years of age. His studies led him to write on the lymphatic system, leading to a public written dispute with William Hunter. In 1753 he demonstrated the communication channels between both lateral and third ventricle of the brain, describing it in a published work in 1797. Since then, these channels have been know as the foramina of Monro. Later analysis of prior publications demonstrate that these foramina were known, although probably not well understood.
The Monro family gave history three anatomists who occupied the chair of Anatomy at the University of Edinburgh for over a century. Alexander Monro Primus (1697 - 1767), Alexander Monro Secundus (1733 - 1817), and Alexander Monro Tertius (1773 - 1859)
Sources:
1. Sharp, J. A. (1961). Alexander Monro secundus and the interventricular foramen. Medical History, 5(1), 83
2. Wu, O. C., Manjila, S., Malakooti, N., & Cohen, A. R. (2012). The remarkable medical lineage of the Monro family: contributions of Alexander primus, secundus, and tertius. Journal of neurosurgery, 116(6), 1337-1346.
3. "The origin of Medical Terms" Skinner, HA; 1970
Original image: Coloured stipple engraving by James Heath (1757–1834), after Henry Raeburn (1756–1823) [Public domain], via Wikimedia Commons
- Details
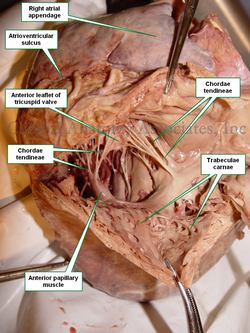
The chordae tendineae, as their Latin name suggests, are tendinous cords found in the right and left ventricles of the heart. These chordae tendineae connect the papillary muscles to the leaflets of the atrioventricular (AV) valves. The vernacular term for these structures is "heart strings".
The function of the chordae tendineae is to limit the freedom of motion of the cusps of the AV valves (tricuspid and mitral), limiting their capacity to "flap" back into the corresponding atrium. Rupture of one or more chordae can cause retrograde flow (reflux or regurgitation) of blood from the ventricle into the atrium, causing cardiac dysfunction.
The chordae tendineae are part of a larger complex of interacting anatomical structures that include the fibrous "skeleton of the heart", the fibrous core of the AV valves, the chordae tendineae, the papillary muscles, and the complex fibrous internal structure of the papillary muscles and the ventricular wall.
The image shows the dissection of a human heart, with the right atrium open. The fan-like shape of the many chordae tendineae is clearly visible, spanning two leaflets. Observe that some chordae tendineae arise directly from the interventricular septum. These are known as the "septal chordae tendineae". Observe the atrioventricular sulcus, and the cardiac apex.
Image property of: CAA.Inc.
- Details
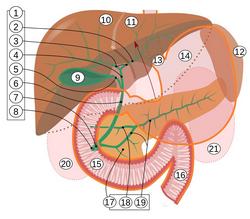
The [common hepatic duct] is one of the components of the extrahepatic hepatobiliary tree that takes bile produced in the liver and transports it to the duodenum, with a storage function in the gallbladder.
The common hepatic duct (CHD) is formed by the junction of the right and left hepatic ducts which bring bile from the right and left functional lobes of the liver respectively. These hepatic ducts converge forming an obtuse angle.
During its trajectory the CHD is found between the layers of the lesser omentum. It has anatomical relations with the proper hepatic artery and the portal vein.
The CHD has an average diameter of 4 to 5 mm and an average length of 3cm (Testut & Latarjet 1931). It ends at the point of origin of the cystic duct which takes bile to the gallbladder. The CHD continues with the common bile duct, which empties into the second portion of the duodenum through the hepatopancreatic ampulla, also known as the Ampulla of Vater.
As with all the components of the hepatobiliary tree, the CHD presents with many anatomical variations. In cases the CHD has been reported with a length of 42 mm, and as short as 3 mm.
Following is the key to the image: 1. Bile ducts: 2. Intrahepatic bile ducts 3. Left and right hepatic ducts, 4. Common hepatic duct 5. Cystic duct 6. Common bile duct 7. Ampulla of Vater 8. Major duodenal papilla 9. Gallbladder 10–11 Right and left lobes of liver 12. Spleen. 13. Esophagus 14. Stomach Small intestine: 15. Duodenum, 16. Jejunum 17. Pancreas: 18: Accessory pancreatic duct, 19: Pancreatic duct. 20–21: Right and left kidneys (silhouette). The anterior border of the liver is lifted superiorly (brown arrow). Gallbladder in longitudinal section, pancreas and duodenum in frontal section. Intrahepatic ducts and stomach in transparency.
Sources:
1. "Tratado de Anatomia Humana" Testut et Latarjet 8 Ed. 1931 Salvat Editores, Spain
2. "Gray's Anatomy" 38th British Ed. Churchill Livingstone 1995
Original image (Public domain) by Jmarchn (Own work) [CC BY-SA 3.0 (http://creativecommons.org/licenses/by-sa/3.0) or GFDL (http://www.gnu.org/copyleft/fdl.html)], via Wikimedia Commons
- Details
The simplest definition of the prefix [pro-] is that it means “forward”. The truth is quite more complicated.
This prefix, used in vernacular English, actually has two different origins and meanings. One arises from the Latin [pro], meaning “on behalf of”, or “in favor of”, and as such we see it in the words proactive, pro-independence, and prohibition.
The second meaning comes from the Greek [πρό] (pr?) meaning “before” and “fore”. This evolved into “in front of” and later to “forward”, which is the main meaning used in medical terminology, as in the words prognosis and prolapse.
- Details
The root term [-gnath-] arises from the Greek word [γνάθος] (gn?thos) meaning “jaw” or “jaw bone”. It is used in medical terms referring to jaw pathology,
- Prognathism or prognathia: The prefix [pro-] means “forward”. A protrusion of the jaw
- Retrognathism or retrognathia: The prefix [retro-] means “posterior”. A posterior displacement caused by lack of development of the jaw
- Micrognathia: The prefix [micro-] means “small”. A small jaw
All these words (prognathism, retrognathism, and micrognathism) are examples of dysmorphism. The accompanying image shows a case of acromegaly with consequent prognathism due to overdevelopment of the jaw.
Note: The links to Google Translate include an icon that will allow you to hear the pronunciation of the word.
Image: By Philippe Chanson and Sylvie Salenave [CC BY 2.0 (http://creativecommons.org/licenses/by/2.0)], via Wikimedia Commons