Medical Terminology Daily (MTD) is a blog sponsored by Clinical Anatomy Associates, Inc. as a service to the medical community. We post anatomical, medical or surgical terms, their meaning and usage, as well as biographical notes on anatomists, surgeons, and researchers through the ages. Be warned that some of the images used depict human anatomical specimens.
You are welcome to submit questions and suggestions using our "Contact Us" form. The information on this blog follows the terms on our "Privacy and Security Statement" and cannot be construed as medical guidance or instructions for treatment.
We have 315 guests online

Jean George Bachmann
(1877 – 1959)
French physician–physiologist whose experimental work in the early twentieth century provided the first clear functional description of a preferential interatrial conduction pathway. This structure, eponymically named “Bachmann’s bundle”, plays a central role in normal atrial activation and in the pathophysiology of interatrial block and atrial arrhythmias.
As a young man, Bachmann served as a merchant sailor, crossing the Atlantic multiple times. He emigrated to the United States in 1902 and earned his medical degree at the top of his class from Jefferson Medical College in Philadelphia in 1907. He stayed at this Medical College as a demonstrator and physiologist. In 1910, he joined Emory University in Atlanta. Between 1917 -1918 he served as a medical officer in the US Army. He retired from Emory in 1947 and continued his private medical practice until his death in 1959.
On the personal side, Bachmann was a man of many talents: a polyglot, he was fluent in German, French, Spanish and English. He was a chef in his own right and occasionally worked as a chef in international hotels. In fact, he paid his tuition at Jefferson Medical College, working both as a chef and as a language tutor.
The intrinsic cardiac conduction system was a major focus of cardiovascular research in the late nineteenth and early twentieth centuries. The atrioventricular (AV) node was discovered and described by Sunao Tawara and Karl Albert Aschoff in 1906, and the sinoatrial node by Arthur Keith and Martin Flack in 1907.
While the connections that distribute the electrical impulse from the AV node to the ventricles were known through the works of Wilhelm His Jr, in 1893 and Jan Evangelista Purkinje in 1839, the mechanism by which electrical impulses spread between the atria remained uncertain.
In 1916 Bachmann published a paper titled “The Inter-Auricular Time Interval” in the American Journal of Physiology. Bachmann measured activation times between the right and left atria and demonstrated that interruption of a distinct anterior interatrial muscular band resulted in delayed left atrial activation. He concluded that this band constituted the principal route for rapid interatrial conduction.
Subsequent anatomical and electrophysiological studies confirmed the importance of the structure described by Bachmann, which came to bear his name. Bachmann’s bundle is now recognized as a key determinant of atrial activation patterns, and its dysfunction is associated with interatrial block, atrial fibrillation, and abnormal P-wave morphology. His work remains foundational in both basic cardiac anatomy and clinical electrophysiology.
Sources and references
1. Bachmann G. “The inter-auricular time interval”. Am J Physiol. 1916;41:309–320.
2. Hurst JW. “Profiles in Cardiology: Jean George Bachmann (1877–1959)”. Clin Cardiol. 1987;10:185–187.
3. Lemery R, Guiraudon G, Veinot JP. “Anatomic description of Bachmann’s bundle and its relation to the atrial septum”. Am J Cardiol. 2003;91:148–152.
4. "Remembering the canonical discoverers of the core components of the mammalian cardiac conduction system: Keith and Flack, Aschoff and Tawara, His, and Purkinje" Icilio Cavero and Henry Holzgrefe Advances in Physiology Education 2022 46:4, 549-579.
5. Knol WG, de Vos CB, Crijns HJGM, et al. “The Bachmann bundle and interatrial conduction” Heart Rhythm. 2019;16:127–133.
6. “Iatrogenic biatrial flutter. The role of the Bachmann’s bundle” Constán E.; García F., Linde, A.. Complejo Hospitalario de Jaén, Jaén. Spain
7. Keith A, Flack M. The form and nature of the muscular connections between the primary divisions of the vertebrate heart. J Anat Physiol 41: 172–189, 1907.
"Clinical Anatomy Associates, Inc., and the contributors of "Medical Terminology Daily" wish to thank all individuals who donate their bodies and tissues for the advancement of education and research”.
Click here for more information
- Details
UPDATED: The word [sphincter] derives from the Greek [σφιγκτήρ] (sfinkt??r), with the same meaning, in turn arising from the Greek word [σφιχτός] (sficht?s) meaning "tight". . The term was originally used by Galen (129AD - 200AD) in the meaning of "to bind tight" or "that which binds tight".
A sphincter is an area of circular muscle fibers that controls a canal or an opening. Rufus named some of them, because of their shape, [orbicularis], a Latin term meaning "circular". An example of this nomenclature are the [orbicularis oculi] and the [orbicularis ori] muscles, the circular muscles of the eye and mouth, respectively.
Some of the so-called "sphincters" in the body are functional sphincters, that is, they control a canal mostly because of their shape, not because of the constrictive action of their circular muscle fibers, such as the ileocecal sphincter or valve, which is normally a one-way valve or a check-valve (shown in the picture)
Other sphincters are true anatomical sphincters, where the number and strength of their circular fibers close off the lumen of the organ, but these are not one-way valves. An example of this type of sphincter is the pylorus.
Images and links public domain, courtesy of: www.bartleby.com
- Details
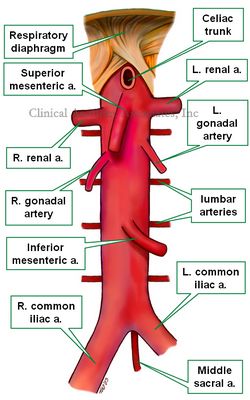
UPDATED: The abdominal aorta is the fourth, last, and most distal portion of the aorta. It begins when the descending aorta passes through the aortic hiatus of the respiratory diaphragm, just about the level of the 11th or 12th thoracic vertebra. It ends inferiorly at the bifurcation of the aorta, anterior to the lower portion of the body of the 4th lumbar vertebra where the abdominal aorta is continuous with the right and left common iliac arteries.
The abdominal aorta gives off a number of paired (bilateral) and unpaired (single) arterial branches. The paired branches are:
• Inferior phrenic arteries: provide blood supply to the respiratory diaphragm
• Renal arteries: Provide blood supply to the kidneys
• Gonadal arteries: Depending on the gender, they are called testicular or ovarian arteries, providing blood supply to the gonads
• Lumbar arteries: There are four pairs of lumbar arteries, which pass posteriorly around the vertebral bodies and provide supply to the spine and the back.
• Suprarenal arteries: These are several minute arteries that provide blood supply to the suprarenal glands. The suprarenal (adrenal) glands also receive several minute arteries that arise from the renal arteries and the inferior phrenic arteries.
The unpaired arterial branches of the abdominal aorta are:
• Celiac trunk: Provides blood supply to the stomach, spleen, liver, and duodenum
• Superior mesenteric artery: Provides blood supply to duodenum, jejunum, ileum, and the right side of the colon
• Inferior mesenteric artery: Provides blood supply to the left side of the colon, and superior aspect of the rectum
• Middle sacral artery: This is the only branch of the aorta that arises from its posterior aspect, it descends providing blood supply to the sacrum and fifth lumbar vertebra
Clinically, the abdominal aorta is divided by the origin of the renal arteries into a suprarenal and an infrarenal segment. This division is important for the surgical treatment of abdominal aortic aneurysms (AAA). To see a AAA, click here.
The suprarenal segment is bound laterally by the crura of the respiratory diaphragm. and its inferior boundary is the superior aspect of the highest renal artery (usually the left renal artery). It has branches that are critical for the blood supply of most of the digestive tract, the celiac trunk and the superior mesenteric artery, plus the inferior phrenic arteries and the suprarenal arteries.
The infrarenal segment includes the renal arteries, the inferior mesenteric artery, gonadal arteries, lumbar arteries, and the middle sacral artery.
Image property of:CAA.Inc.Artist:Victoria G. Ratcliffe
- Details
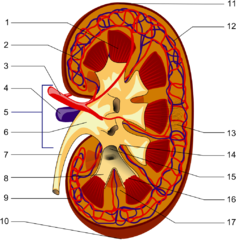
UPDATED: Definition: "A hilum" is the area of an organ where all the structures that enter or leave the organ are found". The term is based on a Latin word meaning something small, or trivial. Also used to describe the small spot on a seed where the seed is attached. The Latin phrase [ne hilum] was used to denote something of no worth or "not at all". In English it would have been similar to "not worth a bean". The plural form for [hilum] is [hila].
In human anatomy the term is used more on the seed attachment meaning. Since a hilum is the area of an organ where all the structures that enter or leave the organ are found, severing the root structures at the level of the hilum detaches the organ from the body. There are several hila in the body:
• Renal hilum: The hilum of the kidney (see item 5 in the accompanying image)
• Lienal hilum: The hilum of the spleen
• Splenic hilum: The hilum of the spleen
• Pulmonary hilum: The hilum of the spleen
• Hepatic hilum: The hilum of the liver. This name is not commonly used and the hepatic hilum is known as the "porta hepatis" meaning the "door to the liver".
There is a wrong version of the term. The word [hilus] is sometimes used and is incorrect. This word was a mistake by the anatomist Bartolomeo Eustachius (c.1520 - 1574) that has continued until today.
Here is the key to the image: Longitudinal section of a kidney. 1-Renal pyramid, 3-Renal artery, 4-Renal vein, 5-Renal hilum, 6-Renal pelvis, 7- Ureter, 8-Minor calyx, 9-Renal capsule, 14-Minor calyx, 15- Major calyx, 16-Renal papilla, 17-Renal column .
Original Image by Piotr Micha? Jaworski; PioM EN DE PL (Own work) [GFDL (http://www.gnu.org/copyleft/fdl.html) or CC-BY-SA-3.0 (http://creativecommons.org/licenses/by-sa/3.0/)], via Wikimedia Commons
- Details
The suffix [-(o)gram] evolved from the Greek word [γράμμα] (gr?mma) , meaning "letter". It was used to denote the written record that was maintained about a patient's ailment. When modern devices that could record an examination, such as an electrocardiograph, the suffix [-ogram] was added to the graphic, so we end up with an electrocardiogram. Today we use it to mean "examination of" with the caveat that some type of written, photographic, digital or drawn record must be left behind. Examples of the use of this suffix are:
- Cholangiogram: Examination of a bile vessel
- Angiogram: Examination of a vessel
- Mammogram: Examination of a breast
- Electrocardiogram: Examination of the electrical activity of the heart. EKG or ECG
- Details
The term [cholecystectomy] is composed by the combined root terms [-chole-] derived from the Greek word [χολή] (cholí) meaning "gall" or "bile, and the root term [-cyst-], also derived from the Greek [κύστη], meaning "bladder". The suffix [-ectomy] results from the combination of two Greek words and means "removal of". For more information of this suffix, click here.
A cholecystectomy is a surgical procedure to remove the gallbladder. It is usually performed because the patient has cholecystolithiasis, a condition where there are calculi (stones) in the gallbladder.
Cholecystectomies were initially made through an "open" procedure, where an incision was done in the abdomen. Today the procedure is performed laparoscopically through small incisions. The first laparoscopic cholecystectomy was performed by Dr. Eric Muhe (1938 - 2005) on September 12, 1985. He was followed by Francois Dubois in 1988, and others. Today with the exception of major emergencies or extremely large gallbladders most cholecystectomies are performed laparoscopically.
The accompanying YouTube video shows a laparoscopic cholecystectomy with a detailed demonstration of the instrumentation used in the procedure, courtesy The Mount Sinai Surgical Film Atlas. Because this video shows a surgical procedure and it is age-restricted. To watch the video you will have to log in to YouTube
Note: The links to Google Translate include an icon that will allow you to hear the Greek or Latin pronunciation of the word.
- Details
This article is part of the series "A Moment in History" where we honor those who have contributed to the growth of medical knowledge in the areas of anatomy, medicine, surgery, and medical research.
John E. Skandalakis, MD, PhD, FACS (1920-2009). Born in Greece, Dr. Skandalakis studied Medicine in Athens. During WWII he fought with the Greek Resistance earning a medal from the Greek government. In the USA Dr. Skandalakis obtained an additional degree in Anatomy, becoming one of the few surgeon-anatomists of our age. An extraordinary teacher, Dr. Skandalakis authored over 300 publications, including journal publications and books1. He is well known for his publications on surgical anatomy related to hernia procedures.
I had the pleasure and the opportunity of meeting and speaking with Dr. John Skandalakis a few times. He always impressed me with his dedication to Clinical Anatomy and his passion for the importance of Anatomy in Surgery. During the 1999 meeting of the American Association of Clinical Anatomists.
In 1992, Dr Skandalakis was awarded the title of "An Immortal" by the Academy of Athens, an award reserved for excellent achievement in the Arts, Sciences, and Humanities. This award has its origins from the time of Plato2.
The Journal of Clinical Anatomy published an "In Remembrance" article on Dr. Skandalakis and his life. I strongly recommend it to anyone who would like to know more about the life and works of Dr. Skandalakis. His picture in this page is a link to The Centers for Surgical Anatomy and Technique of the Emory University School of Medicine.
I was saddened by the news of his passing, but he will be remembered by all those he touched in his life: family, patients, students, and peers. I am also sure that his legacy will go on through his writings, and by those who like me, influence and teach others with his knowledge. I am honored to have met him. Dr. Miranda
Original image of Dr. John E. Skandalakis courtesy of the the Centers for Surgical Anatomy and Technique.
Sources:
1. "Obituary: Dr. John Skandalakis, 1920-2009" Jones, G. Hernia (2010) 14: 79-80
2. "In Remembrance: John Elias Skandalakis,MD,PhD,FACS (1920–2009)Loukas,M; Colborn,L; Tubbs: RS Clin Anat 23:332–334 (2010)