Medical Terminology Daily (MTD) is a blog sponsored by Clinical Anatomy Associates, Inc. as a service to the medical community. We post anatomical, medical or surgical terms, their meaning and usage, as well as biographical notes on anatomists, surgeons, and researchers through the ages. Be warned that some of the images used depict human anatomical specimens.
You are welcome to submit questions and suggestions using our "Contact Us" form. The information on this blog follows the terms on our "Privacy and Security Statement" and cannot be construed as medical guidance or instructions for treatment.
We have 1513 guests online

Jean George Bachmann
(1877 – 1959)
French physician–physiologist whose experimental work in the early twentieth century provided the first clear functional description of a preferential interatrial conduction pathway. This structure, eponymically named “Bachmann’s bundle”, plays a central role in normal atrial activation and in the pathophysiology of interatrial block and atrial arrhythmias.
As a young man, Bachmann served as a merchant sailor, crossing the Atlantic multiple times. He emigrated to the United States in 1902 and earned his medical degree at the top of his class from Jefferson Medical College in Philadelphia in 1907. He stayed at this Medical College as a demonstrator and physiologist. In 1910, he joined Emory University in Atlanta. Between 1917 -1918 he served as a medical officer in the US Army. He retired from Emory in 1947 and continued his private medical practice until his death in 1959.
On the personal side, Bachmann was a man of many talents: a polyglot, he was fluent in German, French, Spanish and English. He was a chef in his own right and occasionally worked as a chef in international hotels. In fact, he paid his tuition at Jefferson Medical College, working both as a chef and as a language tutor.
The intrinsic cardiac conduction system was a major focus of cardiovascular research in the late nineteenth and early twentieth centuries. The atrioventricular (AV) node was discovered and described by Sunao Tawara and Karl Albert Aschoff in 1906, and the sinoatrial node by Arthur Keith and Martin Flack in 1907.
While the connections that distribute the electrical impulse from the AV node to the ventricles were known through the works of Wilhelm His Jr, in 1893 and Jan Evangelista Purkinje in 1839, the mechanism by which electrical impulses spread between the atria remained uncertain.
In 1916 Bachmann published a paper titled “The Inter-Auricular Time Interval” in the American Journal of Physiology. Bachmann measured activation times between the right and left atria and demonstrated that interruption of a distinct anterior interatrial muscular band resulted in delayed left atrial activation. He concluded that this band constituted the principal route for rapid interatrial conduction.
Subsequent anatomical and electrophysiological studies confirmed the importance of the structure described by Bachmann, which came to bear his name. Bachmann’s bundle is now recognized as a key determinant of atrial activation patterns, and its dysfunction is associated with interatrial block, atrial fibrillation, and abnormal P-wave morphology. His work remains foundational in both basic cardiac anatomy and clinical electrophysiology.
Sources and references
1. Bachmann G. “The inter-auricular time interval”. Am J Physiol. 1916;41:309–320.
2. Hurst JW. “Profiles in Cardiology: Jean George Bachmann (1877–1959)”. Clin Cardiol. 1987;10:185–187.
3. Lemery R, Guiraudon G, Veinot JP. “Anatomic description of Bachmann’s bundle and its relation to the atrial septum”. Am J Cardiol. 2003;91:148–152.
4. "Remembering the canonical discoverers of the core components of the mammalian cardiac conduction system: Keith and Flack, Aschoff and Tawara, His, and Purkinje" Icilio Cavero and Henry Holzgrefe Advances in Physiology Education 2022 46:4, 549-579.
5. Knol WG, de Vos CB, Crijns HJGM, et al. “The Bachmann bundle and interatrial conduction” Heart Rhythm. 2019;16:127–133.
6. “Iatrogenic biatrial flutter. The role of the Bachmann’s bundle” Constán E.; García F., Linde, A.. Complejo Hospitalario de Jaén, Jaén. Spain
7. Keith A, Flack M. The form and nature of the muscular connections between the primary divisions of the vertebrate heart. J Anat Physiol 41: 172–189, 1907.
"Clinical Anatomy Associates, Inc., and the contributors of "Medical Terminology Daily" wish to thank all individuals who donate their bodies and tissues for the advancement of education and research”.
Click here for more information
- Details
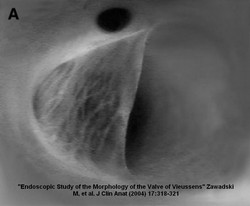
The eponymic “valve of Vieussens” is a venous valve found at the most proximal portion (or beginning) of the coronary sinus. The valve was first described by Raymond de Vieussens and thus carries its name.
Venous valves are common on peripheral veins but they tend not to be present on intraabdominal and intrathoracic veins, with some exceptions. These valves are form by thin veil-like reduplications of the venous endothelium.
Zawadzki, et al (2004) demonstrated in an endoscopic study of the valve of Vieussens that it is present in 78% of the cases and that the valve can be single, double, and even triple. The morphology of this particular valve is of interest as there are some cardiac catheterization procedures that may attempt to pass a retrograde catheter or fluid from the coronary sinus into the great cardiac vein.
Sources:
1. “Endoscopic Study of the Morphology of Vieussens Valve” Zawadzki, M. et al Clinical Anatomy (2004) 17:318 –321
2. “The valve of Vieussens: an important cause of difficulty in advancing catheters into the cardiac veins” Corcoran, SJ J Cardiovasc Electrophysiol. 1999 Jun;10(6):804-8
3. “Valve of Vieussens: An obstacle for left ventricular lead placement” Sthromer, B Can J Cardiol. Sep 2008; 24(9): e63
- Details
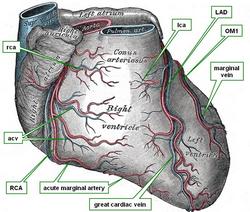
The marginal veins are usually two (sometimes three) venous branches each which run along or parallel with the obtuse marginal arteries. They represent the venous return from the anterolateral aspect of the left ventricular wall.
The first (obtuse) marginal vein usually anastomoses with the great cardiac vein just before the great cardiac vein empties into the coronary sinus. The other obtuse marginal veins may enter the coronary sinus directly
Sources:
1. "Gray's Anatomy" 38th British Ed. Churchill Livingstone 1995
2. “Variable anatomy of the right coronary artery supply to the left ventricle” Adams, J. Treasure, T. Thorax 1985;40:618-623
4. "Anatomy of the Human Body" Henry Gray 1918. Philadelphia: Lea & Febiger
Image modified by CAA, Inc. Original image courtesy of bartleby.com
- Details
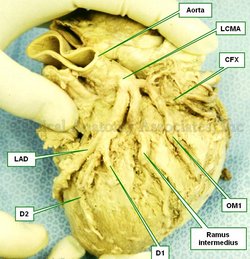
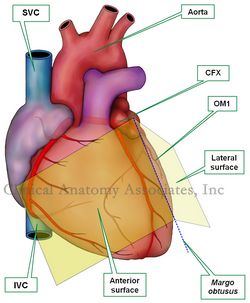
This is the name given to a particular anatomical variation of the bifurcation of the left coronary artery (LMCA). Normally the LMCA bifurcates giving origin to the circumflex artery (CFX) and the anterior interventricular artery, also known as the left anterior descending artery (LAD).
In the case of the “ramus intermedius” variation, the LCMA trifurcates, that is, forks into three branches: an LAD, a CFX and an intermediate branch that provides blood supply to the anterolateral aspect of the left ventricular surface and/or the obtuse margin of the heart. The ramus intermedius may take one of two directions. It may behave like a diagonal branch (D1, D2) of the LAD or as an obtuse marginal artery (OM1).
The ramus intermedius anatomical variation is quite common and literature states that it may be present in 20-33% of the cases.
One of my pet peeves (see my top pet peeve here) is that most medical industry providers as well as many surgeons and physicians call this anatomical variation a “ramus”. You see, the Latin term [ramus] means “branch” and by itself is not descriptive. The proper name is the Latin term “ramus intermedius” which means “the intermediate branch”.
Image property of CAA,Inc.
- Details
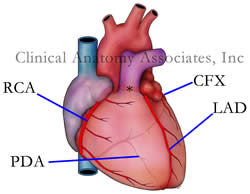
The left coronary artery, sometimes called the [left main coronary artery] or LMCA, is a short artery that arises from the aortic root at the left posterior coronary sinus of Valsalva, usually below the sinotubular junction.
Its length is on average 1.3 cm, although it can be shorter. The LMCA courses between the left atrial appendage and the posterior aspect of the pulmonary trunk. The LMCA provides blood supply to almost 69% of the heart, making it most important in coronary blood supply to the heart. This apparently goes against the concept of coronary dominance if the concept is not clearly understood. You could have a "right dominant heart" and still have the LMCA provide blood supply to more than 50% of the heart.
The left coronary artery bifurcates giving origin to two branches: the circumflex artery (CFX) and the left anterior descending artery (LAD). Each one of these arteries gives origin to several named branches and you can click on the links to follow each one.
The left coronary artery has several anatomical variations, including one where it does not exist and the CFX and LAD arise separately from the aorta. In another common variation (25-33%) the aorta trifurcates giving rise to a [ramus intermedius]
Sources:
1 "Tratado de Anatomia Humana" Testut et Latarjet 8 Ed. 1931 Salvat Editores, Spain
2. "Gray's Anatomy" 38th British Ed. Churchill Livingstone 1995
3. “Anatomical variations in the left coronary artery and its branches” Hosapatna, M et al. Singapore Med J 2013; 54(1) : 49
4. "Quantitative study on the size of coronary artery supplying areas postmortem" Kalbfleisch H. Am Heart J 1977; 94:183-8.
Image property of: CAA.Inc. Artist: Victoria G. Ratcliffe
- Details
The obtuse marginal arteries are two (sometimes three) branches that arise of the circumflex artery and descend towards the cardiac apex with varying lengths. The first obtuse marginal artery (OM1) is usually found on or close to the obtuse margin of the heart, also known as the “margo obtusus”
The first obtuse marginal artery (OM1) along with the acute marginal artery are used to denote the lower portion of the heart and the location of the cardiac apex in coronary angiography.
There is an anatomical variation of the origin of OM1 where this artery arises at the bifurcation of the left coronary artery where this artery takes the name “ramus intermedius”
Sources:
1. "Gray's Anatomy" 38th British Ed. Churchill Livingstone 1995
2. “Variable anatomy of the right coronary artery supply to the left ventricle” Adams, J. Treasure, T. Thorax 1985;40:618-623
4. "Anatomy of the Human Body" Henry Gray 1918. Philadelphia: Lea & Febiger
Image modified by CAA, Inc. Original image courtesy of bartleby.com
- Details
The term "obtuse margin" refers to the superolateral border of the anterior surface of the heart. It is also known by its Latin name [margo obtusus].
The name of this border or margin of the heart is quite descriptive. If you observe the accompanying image, the angle formed between the anterior or sternocostal surface of the heart with the left lateral or left pulmonary surface of the heart, you can see that the angle between these two surfaces is more than 90 degrees, therefore an "obtuse" angle. The corresponding border between these two surfaces has to be called the "obtuse margin"!
In relation to the obtuse margin of the heart we can usually find the first branch that arises from the circumflex artery. This artery is called Obtuse Marginal 1 or OM1.
Click on the image for a larger depiction. Here is a link to an article on the "acute margin" of the heart.
Sources:
1 "Tratado de Anatomia Humana" Testut et Latarjet 8 Ed. 1931 Salvat Editores, Spain