
Medical Terminology Daily (MTD) is a blog sponsored by Clinical Anatomy Associates, Inc. as a service to the medical community. We post anatomical, medical or surgical terms, their meaning and usage, as well as biographical notes on anatomists, surgeons, and researchers through the ages. Be warned that some of the images used depict human anatomical specimens.
You are welcome to submit questions and suggestions using our "Contact Us" form. The information on this blog follows the terms on our "Privacy and Security Statement" and cannot be construed as medical guidance or instructions for treatment.
We have 1531 guests online

Jean George Bachmann
(1877 – 1959)
French physician–physiologist whose experimental work in the early twentieth century provided the first clear functional description of a preferential interatrial conduction pathway. This structure, eponymically named “Bachmann’s bundle”, plays a central role in normal atrial activation and in the pathophysiology of interatrial block and atrial arrhythmias.
As a young man, Bachmann served as a merchant sailor, crossing the Atlantic multiple times. He emigrated to the United States in 1902 and earned his medical degree at the top of his class from Jefferson Medical College in Philadelphia in 1907. He stayed at this Medical College as a demonstrator and physiologist. In 1910, he joined Emory University in Atlanta. Between 1917 -1918 he served as a medical officer in the US Army. He retired from Emory in 1947 and continued his private medical practice until his death in 1959.
On the personal side, Bachmann was a man of many talents: a polyglot, he was fluent in German, French, Spanish and English. He was a chef in his own right and occasionally worked as a chef in international hotels. In fact, he paid his tuition at Jefferson Medical College, working both as a chef and as a language tutor.
The intrinsic cardiac conduction system was a major focus of cardiovascular research in the late nineteenth and early twentieth centuries. The atrioventricular (AV) node was discovered and described by Sunao Tawara and Karl Albert Aschoff in 1906, and the sinoatrial node by Arthur Keith and Martin Flack in 1907.
While the connections that distribute the electrical impulse from the AV node to the ventricles were known through the works of Wilhelm His Jr, in 1893 and Jan Evangelista Purkinje in 1839, the mechanism by which electrical impulses spread between the atria remained uncertain.
In 1916 Bachmann published a paper titled “The Inter-Auricular Time Interval” in the American Journal of Physiology. Bachmann measured activation times between the right and left atria and demonstrated that interruption of a distinct anterior interatrial muscular band resulted in delayed left atrial activation. He concluded that this band constituted the principal route for rapid interatrial conduction.
Subsequent anatomical and electrophysiological studies confirmed the importance of the structure described by Bachmann, which came to bear his name. Bachmann’s bundle is now recognized as a key determinant of atrial activation patterns, and its dysfunction is associated with interatrial block, atrial fibrillation, and abnormal P-wave morphology. His work remains foundational in both basic cardiac anatomy and clinical electrophysiology.
Sources and references
1. Bachmann G. “The inter-auricular time interval”. Am J Physiol. 1916;41:309–320.
2. Hurst JW. “Profiles in Cardiology: Jean George Bachmann (1877–1959)”. Clin Cardiol. 1987;10:185–187.
3. Lemery R, Guiraudon G, Veinot JP. “Anatomic description of Bachmann’s bundle and its relation to the atrial septum”. Am J Cardiol. 2003;91:148–152.
4. "Remembering the canonical discoverers of the core components of the mammalian cardiac conduction system: Keith and Flack, Aschoff and Tawara, His, and Purkinje" Icilio Cavero and Henry Holzgrefe Advances in Physiology Education 2022 46:4, 549-579.
5. Knol WG, de Vos CB, Crijns HJGM, et al. “The Bachmann bundle and interatrial conduction” Heart Rhythm. 2019;16:127–133.
6. “Iatrogenic biatrial flutter. The role of the Bachmann’s bundle” Constán E.; García F., Linde, A.. Complejo Hospitalario de Jaén, Jaén. Spain
7. Keith A, Flack M. The form and nature of the muscular connections between the primary divisions of the vertebrate heart. J Anat Physiol 41: 172–189, 1907.
"Clinical Anatomy Associates, Inc., and the contributors of "Medical Terminology Daily" wish to thank all individuals who donate their bodies and tissues for the advancement of education and research”.
Click here for more information
- Details
The root term -blephar-] arises from the Greek [βλέφαρο]meaning "eyelid".
It is used in many medical terms such as:
- Blepharoplasty: The suffix [-(o)plasty] means "reshaping". The surgical reshaping of an eyelid
- Blepharitis: The suffix [-itis] means "inflammation" or "infection". The inflammation of an eyelid
- Blepharoptosis: The suffix [-(o)ptosis] means "to sag" or "to "fall". A sagging or drooping eyelid
Note: The links to Google Translate in these articles include an icon that will allow you to hear the Greek or Latin pronunciation of the word.
Image courtesy of Kami Parsa, MD. Original image link courtesy of Wikipedia
- Details
The word [cathedra] is Greek, from [καθέδρα] meaning "a high chair", a "teacher's chair" or a "throne". The term was later accepted into Latin with the same meaning.
In the early pre-Vesalian days of anatomy, the teachers would seat in a high-chair or cathedra from where they would read the anatomy from a book while a prosector or demonstrator would dissect, expose and point to the structures. The professor would not consider coming down from the cathedra to discuss the anatomy shown. This was changed by Andreas Vesalius who did the dissections and demonstrations himself, using the books as reference or to prove a point.
The term cathedra has been brought to our times, where we refer to the position at the head of a group as the "Chair": Chair of the Science Department, Chair of Surgery, etc.
The word cathedra was used to refer to a Bishop's chair in a church, so that large churches (which had a bishop) are now known as [cathedrals]. It is also said that someone of authority speaking in uncontestable terms is speaking ex-cathedra (from the chair)
In other languages the term "cathedratic" means a teacher in a high position, while in English the term refers to a Bishop speaking from the chair.
The image in this article is a close up of the title page of Mondino de Luzzi’s “Anothomia Corporis Humani” published in 1478. The person on the image could be Alessandra Giliani (1307 - 1326) who is at the foot of the cathedra following the directions of Mondino de Luzzi. Click on the image for a complete depiction of the title page.
Original image courtesy of NLM
- Details
The term [nystagmus] is derived from the Greek word [νυσταγμένος], (nystagm?nos) meaning "sleepy" or "dizzy". It refers to the sensation of dizziness when you are just awakening from a deep sleep.
In medical terminology nystagmus refers to the rapid, usually lateral, movement of the eyes. This movement has a slower component that moves en eye to one side with a secondary rapid component that brings the eye to the starting point. Nystagmus eye movement is usually bilateral and can be unilateral in rare cases.
Nystagmus is a normal capability of the human visual system where the eyes move slightly to change the location of an image on the retina to avoid fatigue of the retinal components. In some individuals this movement is quite visible but it does not cause a problem and is called physiological or congenital nystagmus as shown in the video..
When nystagmus is pathological it can be the cause for vertigo, as the patient feels that the world is moving, when only the eyes are doing so. This can be caused by a pathology in the abducens nerve system.
Nystagmus can be triggered by using warm fluids in the external ear that will cause flow of the fluid in the semicircular canals of the inner ear. You can also see it if you turn a person around in a swiveling chair for a few turns and then stop and watch their eyes. You will see the rapid nystagmus movement of the eye. If you do this experiment, please be careful, as a person with nystagmus will have poor balance and they can fall with potential for injury.
Thanks to Lashkyrie for the use of her video on YouTube.
Note: The links to Google Translate include an icon that will allow you to hear the Greek or Latin pronunciation of the word.
- Details
The midclavicular line is one of the surface reference lines used in surface anatomy of the thorax.
It is a parasagittal vertical plane that passes halfway through the body of the clavicle. The lateral portion of the clavicle is close to the highest point of the shoulder joint (the acromioclavicular joint), while the head (medial aspect) of the clavicle is found just lateral to the jugular notch of the sternum, a depression in the superior aspect of the sternal manubrium.
Although it was originally used as a thoracic reference point, the continuation of the midclavicular line into the abdomen is used today as a reference for laparoscopic procedures, to indicate the location where a trocar must be introduced into the abdomen. As an example, in a laparoscopic cholecystectomy, one of the four trocars (in this case a 5mm trocar) is introduced into the abdomen on the right midclavicular line four fingerbreadths inferior to the costal margin (the lower border of the ribs). This trocar is used to manipulate the gallbladder and is placed in the gallbladder infundibulum.
It is also one of the lines used to describe the abdominal regions.
Sources:
1. "Clinical Anatomy" Brantigan, OC 1963 McGraw Hill
2. "Tratado de Anatomia Humana" Testut et Latarjet 8th Ed. 1931 Salvat Editores, Spain
3. Davis, Gwilym G. "Applied Anatomy: The Construction of the Human Body Considered in Relation to Its Functions, Diseases, and Injuries"; Philadelphia: J.B. Lippincott Co., 1910
Image modified from the original Davis, 1910
- Details
The transpyloric plane (also called the transpyloric line) is one of the surface reference lines used in surface anatomy. It is one of the lines used to describe the abdominal regions.
It is a horizontal or transverse plane located halfway between the jugular notch of the sternum, a depression in the superior aspect of the sternal manubrium, and the superior aspect of the symphysis pubis.
The transpyloric plane crosses the body of the first lumbar vertebra and approximates the course and location of the pancreas. The plane also transects the kidney horizontally in half at about the region of the renal hilum. This plane also passes through the origin of the superior mesenteric artery, the body of the gallbladder, and of course through the pylorus of the stomach, from whence the name of this plane arises.
To be precise, the pylorus will be found on or slightly above the transpyloric plane, and slightly to the right of the midline
Sources:
1. "Clinical Anatomy" Brantigan, OC 1963 McGraw Hill
2. "Tratado de Anatomia Humana" Testut et Latarjet 8th Ed. 1931 Salvat Editores, Spain
3. Davis, Gwilym G. "Applied Anatomy: The Construction of the Human Body Considered in Relation to Its Functions, Diseases, and Injuries"; Philadelphia: J.B. Lippincott Co., 1910
Image modified from the original Davis, 1910
- Details
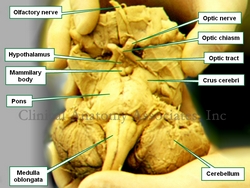
Brainstem. Anteroinferior view
The anatomical term crus cerebri is Latin. The term [crus] means "pillar" or "leg", and [cerebri] means "brain", thus it means the "pillars of the brain" or "the brain legs".
It refers to the anterior view of the midbrain or mesencephalon. There are two slightly divergent columns or pillars separated by the interpeduncular fossa, a space or region that contains in its superior aspect the mammillary bodies. These two columns are also known as the "cerebral peduncles".
The interpeduncular fossa is a dilated region of the subarachnoid space and as such it is a cistern called the "interpeduncular cistern". The oculomotor nerve (third cranial nerve) appears on the lateral aspect of the interpeduncular fossa.
The trochlear nerve (4th cranial nerve) wraps around the lateral aspect of each crura cerebri on its way towards the eye.
Image property of:CAA.Inc.




