Medical Terminology Daily (MTD) is a blog sponsored by Clinical Anatomy Associates, Inc. as a service to the medical community. We post anatomical, medical or surgical terms, their meaning and usage, as well as biographical notes on anatomists, surgeons, and researchers through the ages. Be warned that some of the images used depict human anatomical specimens.
You are welcome to submit questions and suggestions using our "Contact Us" form. The information on this blog follows the terms on our "Privacy and Security Statement" and cannot be construed as medical guidance or instructions for treatment.
We have 727 guests and no members online

Jean George Bachmann
(1877 – 1959)
French physician–physiologist whose experimental work in the early twentieth century provided the first clear functional description of a preferential interatrial conduction pathway. This structure, eponymically named “Bachmann’s bundle”, plays a central role in normal atrial activation and in the pathophysiology of interatrial block and atrial arrhythmias.
As a young man, Bachmann served as a merchant sailor, crossing the Atlantic multiple times. He emigrated to the United States in 1902 and earned his medical degree at the top of his class from Jefferson Medical College in Philadelphia in 1907. He stayed at this Medical College as a demonstrator and physiologist. In 1910, he joined Emory University in Atlanta. Between 1917 -1918 he served as a medical officer in the US Army. He retired from Emory in 1947 and continued his private medical practice until his death in 1959.
On the personal side, Bachmann was a man of many talents: a polyglot, he was fluent in German, French, Spanish and English. He was a chef in his own right and occasionally worked as a chef in international hotels. In fact, he paid his tuition at Jefferson Medical College, working both as a chef and as a language tutor.
The intrinsic cardiac conduction system was a major focus of cardiovascular research in the late nineteenth and early twentieth centuries. The atrioventricular (AV) node was discovered and described by Sunao Tawara and Karl Albert Aschoff in 1906, and the sinoatrial node by Arthur Keith and Martin Flack in 1907.
While the connections that distribute the electrical impulse from the AV node to the ventricles were known through the works of Wilhelm His Jr, in 1893 and Jan Evangelista Purkinje in 1839, the mechanism by which electrical impulses spread between the atria remained uncertain.
In 1916 Bachmann published a paper titled “The Inter-Auricular Time Interval” in the American Journal of Physiology. Bachmann measured activation times between the right and left atria and demonstrated that interruption of a distinct anterior interatrial muscular band resulted in delayed left atrial activation. He concluded that this band constituted the principal route for rapid interatrial conduction.
Subsequent anatomical and electrophysiological studies confirmed the importance of the structure described by Bachmann, which came to bear his name. Bachmann’s bundle is now recognized as a key determinant of atrial activation patterns, and its dysfunction is associated with interatrial block, atrial fibrillation, and abnormal P-wave morphology. His work remains foundational in both basic cardiac anatomy and clinical electrophysiology.
Sources and references
1. Bachmann G. “The inter-auricular time interval”. Am J Physiol. 1916;41:309–320.
2. Hurst JW. “Profiles in Cardiology: Jean George Bachmann (1877–1959)”. Clin Cardiol. 1987;10:185–187.
3. Lemery R, Guiraudon G, Veinot JP. “Anatomic description of Bachmann’s bundle and its relation to the atrial septum”. Am J Cardiol. 2003;91:148–152.
4. "Remembering the canonical discoverers of the core components of the mammalian cardiac conduction system: Keith and Flack, Aschoff and Tawara, His, and Purkinje" Icilio Cavero and Henry Holzgrefe Advances in Physiology Education 2022 46:4, 549-579.
5. Knol WG, de Vos CB, Crijns HJGM, et al. “The Bachmann bundle and interatrial conduction” Heart Rhythm. 2019;16:127–133.
6. “Iatrogenic biatrial flutter. The role of the Bachmann’s bundle” Constán E.; García F., Linde, A.. Complejo Hospitalario de Jaén, Jaén. Spain
7. Keith A, Flack M. The form and nature of the muscular connections between the primary divisions of the vertebrate heart. J Anat Physiol 41: 172–189, 1907.
"Clinical Anatomy Associates, Inc., and the contributors of "Medical Terminology Daily" wish to thank all individuals who donate their bodies and tissues for the advancement of education and research”.
Click here for more information
- Details
This article is part of the series "A Moment in History" where we honor those who have contributed to the growth of medical knowledge in the areas of anatomy, medicine, surgery, and medical research.

John Marshall (1818 – 1891)
John Marshall (1818 – 1891) British anatomist and surgeon. Initially, he apprenticed with Dr. Wales in Wisbech. In 1838 he entered the University College, London, where he studied with William Sharpey (1802 – 1880), who was then teaching physiology. In 1849 Marshall became a Fellow of the Royal College of Surgeons of England.
In 1845 he became a demonstrator of anatomy at University College, London and in 1847 with the help of Jones Quain (1796 – 1865) and William Sharpey he was appointed as assistant surgeon.
Marshall was appointed professor of surgery at University College in 1866, and in 1884 he was appointed consulting surgeon to University College Hospital.
He was known as a great artist and used his abilities to teach anatomy with the help of blackboards. He lectured on anatomy to art students, and one of his books is titled “Anatomy for Artists” (London, 1878), which was received with great enthusiasm by his art students.
John Marshall wrote several books and works, mentioned in the “Sources” section of this article, but he is probably better known for his association with the eponymic “Ligament of Marshall”. In 1850, he published a detailed description (36 pages) of the embryology of the cardinal veins, the superior vena cava, and the presence of a persistent “left superior vena cava” with a description of the oblique vein of the left atrium, the obliterated Duct of Cuvier, and the fold of pericardium over this duct that today carries his name.
The paper was published in the journal “Philosophical Transactions of the Royal Society”, and the title was “On the Development of the Great Anterior Veins Man and Mammalia; including an Account of certain remnants of Fœtal Structure found in the Adult, a Comparative View of these Great Veins the different and an Analysis of their occasional peculiarities in the Human Subject”. The sketches that accompany this seminal paper were drawn by him.
If you are interested in reading this paper, it is available online at the Royal Society website. For the actual publication in PDF format, click here.
Marshall also is recognized for being one of the first to use electrocautery in surgery, as well as being a pioneer in the removal of lower extremity varicose veins. He was the first to demonstrate that cholera can be spread through contaminated drinking water.
The image shows the ligament of Marshall (yellow arrow), the left pulmonary artery (LPA), and the left superior pulmonary vein (LSPV).
Personal note: My thanks to an attendee to one of my cardiovascular lectures. He asked who was Marshall of the "ligament of Marshall:... Here is the answer. Dr. Miranda.
Sources and publications:
1. “A Description of the Human Body, its Structure and Functions” London, 1860, 4to, with folio plates; 4th ed. 1883.
2. “Anatomy for Artists” London, 1878, royal 8vo; 2nd ed. 1883; 3rd edit. 1890.
3. “A Rule of Proportion for the Human Figure” 1878, fol.
4 “A Series of Life-size Anatomical Diagrams” seven sheets.
5. “Physiological Diagrams” life size, eleven sheets.
6. “On the Relations between the Weight of the Brain and its Parts, and the Stature and Mass of the Body” 1892, J Anat Physiol
7. “The Brain of the late George Grote” 1892, J Anat Phys
8. “On the Development of the Great Anterior Veins Man and Mammalia; including an Account of certain remnants of Fœtal Structure found in the Adult, a Comparative View of these Great Veins the different and an Analysis of their occasional peculiarities in the Human Subject” 1850 Phil Trans R Soc 140:133 - 170
9. Portrait of J. Marshall by Alphonse Legros, Courtesy of Wikipedia. Public Domain.
- Details
This article is part of the series "A Moment in History" where we honor those who have contributed to the growth of medical knowledge in the areas of anatomy, medicine, surgery, and medical research.

G.E. Rindfleisch (1836 – 1908)
Georg Eduard Von Rindfleisch (1836 – 1908), German pathologist and histologist of Bavarian nobility ancestry. Rindfleisch studied medicine in Würzburg, Berlin, and Heidelberg, earning his MD in 1859 with the thesis “De Vasorum Genesi” (on the generation of vessels) under the tutelage of Rudolf Virchow (1821 - 1902). He then continued as a assistant to Virchow in a newly founded institute in Berlin. He then moved to Breslau in 1861 as an assistant to Rudolf Heidenhain (1834–1897), becoming a professor of pathological anatomy. In 1865 he became full professor in Bonn and in 1874 in Würzburg, where a new pathological institute was built according to his design (completed in 1878), where he worked until his retirement in 1906.
He was the first to describe the inflammatory background of multiple sclerosis in 1863, when he noted that demyelinated lesions have in their center small vessels that are surrounded by a leukocyte inflammatory infiltrate.
After extensive investigations, he suspected an infectious origin of tuberculosis - even before Robert Koch's detection of the tuberculosis bacillus in 1892. Rindfleisch 's special achievement is the description of the morphologically conspicuous macrophages in typhoid inflammation. His distinction between myocardial infarction and myocarditis in 1890 is also of lasting importance.
Associated eponyms
"Rindfleisch's folds": Usually a single semilunar fold of the serous surface of the pericardium around the origin of the aorta. Also known as the plica semilunaris aortæ.
"Rindfleisch's cells": Historical (and obsolete) name for eosinophilic leukocytes.
Personal note: G. Rindfleisch’s book “Traité D' Histologie Pathologique” 2nd edition (1873) is now part of my library. This book was translated from German to French by Dr. Frédéric Gross (1844-1927) , Associate Professor of the Medicine Faculty in Nancy, France. The book is dedicated to Dr. Theodore Billroth (1829-1894), an important surgeon whose pioneering work on subtotal gastrectomies paved the way for today’s robotic bariatric surgery. Dr. Miranda.
Sources:
1. "Stedmans Medical Eponyms" Forbis, P.; Bartolucci, SL; 1998 Williams and Wilkins
2. "Rindfleisch, Georg Eduard von (bayerischer Adel?)" Deutsche Biographie
3. "The pathology of multiple sclerosis and its evolution" Lassmann H. (1999) Philos Trans R Soc Lond B Biol Sci. 354 (1390): 1635–40.
4. “Traité D' Histologie Pathologique” G.E.
Rindfleisch 2nd Ed (1873) Ballieres et Fils. Paris, Translated by F Gross.
- Details
"Thou to health and vigor should attain
Shun mighty cares, all anger deem profane
From heavy suppers and much wine abstain;
Nor trivial count it after pompous fare
To rise from the table and take to the air.
Spurn idle noonday slumbers, nor delay
The urgent call of nature to obey.
These rules if thou wilt follow to the end
Thy life to greater length thou may extend"
Cover page of Regimen Sanitatis Salernitatum c. 1480
The original poem is written in Latin and is part of the book "Regimen Sanitatis Salernitarum" published in 1480. This book contains articles and poems by Afflacius, Bartholomeus, Copho, Ferrarius, Petronius, Johannes Platearius, and Trotula. The editor of the book was Arnold de Villa Nova. It was later translated into English.
The author of the book was Constantinus Africanus of Carthage (1020-1087). His birth and original religion is in question, some stating that he was a Sarracen, and therefore born as a Muslim. He traveled extensively in Egypt, Greece, Italy, and India. His ability to read and speak Arabic, Latin, Greek, and other languages, helped him later to be considered one of the important translators of medical books bringing lost Latin and Greek knowledge in books from Arab countries into Europe.
After arriving in Salerno, Constantinus became a monk and dedicated his life to the publication of medical translation, not hesitating to call other's works as his own.
It is considered one of the two great publications of the School of Salerno in the Medieval Ages, the other one being the "Compendium Salernitatus"
More on this wonderful book here.
Source:
"Medieval and Renaissance Medicine" B.L. Gordon 1959 Philosophical Library Inc. USA
- Details
This article is part of the series "A Moment in History" where we honor those who have contributed to the growth of medical knowledge in the areas of anatomy, medicine, surgery, and medical research.

Folder of "Sutures in Ancient Surgery"
During a recent 2024 lecture I delivered to a group of engineers at Medtronic, I met with Jack Kennedy, an engineer, past student, and a good friend. Jack and I share a passion for medical history. He has a very interesting collection of antique sutures and books related to the topic. He gifted me a collection of antique photographic prints in a leather-like folder with gilded letters. The name of the work is “Sutures in Ancient Surgery”. Jack was kind enough to sign and dedicate this gift that now holds an important place in my library.
For those who know me, I cannot have a book without looking into its history. What I found was incredible! The findings are in the following areas and topics:
- The history of the Davis and Geck suture company.
2. Lejaren à Hillier, main photographer of “Sutures in Ancient Surgery”
3. The content of the publication, images, and controversy
4. Missing prints
1. The history of the Davis & Geck company
Davis & Geck (D&G) was founded in 1909 by Charles T. Davis and Fred A. Geck, along with Frank D. Bradeen, and Benjamin F. Hirsch. Interestingly, Fred Geck left the company only a few months after its formation, but the company kept his name.
Located in Brooklyn, NY., the company specialized in the development and manufacture of surgical sutures along with various other medical products. Over the years the company changed ownership and has changed its name a couple of times. In 1930, the company was acquired by American Cyanamid after a trial between Charles Davis and his wife. This particular spot in the company’s history includes a murder, prison, lovers, and a trial. If you are interested, read the story of the company at UConn’s and SNAC web pages (see “sources”).
D&G was acquired by Sherwood, and later by the Tyco Corporation where it was renamed Syneture. Tyco Healthcare became Covidien, Ltd., which was later acquired by Medtronic, where it is today.
In 1970 Davis & Geck introduced Dexon, the first synthetic absorbable suture, followed shortly by Ethicon (J&J) sutures with Vicryl. Since then, research and development in the Medtronic line of sutures makes this company one of the world leaders in wound closure.
2. Lejaren à Hillier, main photographer of “Sutures in Ancient Surgery”
Lejaren à Hillier (1880-1969), was born in Milwaukee. He studied at the School of the Chicago Art Institute; his interest was classical fine arts. His studies and activities drew him to experimenting with photography and novel techniques for the times, where he mixed photography and painting. He became a famous commercial photographer.
One of his most exciting works was that of “tableaux vivants” (living portraits), where he would stage actors and innovative lighting techniques to represent scenes that he would later edit with paintings or use different photographic development techniques to obtain the appropriate mood. His work soon caught the attention of companies that used these tableaux vivants in commercial printings for brochures or newspapers.
Hillier was approached by D&G and the project of “Sutures in Ancient Surgery” was born. Starting in 1927 and all trough 1950, D&G sales representatives would present their customers (physicians and surgeons) with the “latest” image, ensuring an open door when they showed up at the doctor’s office. The doctors were also presented with a leather-like folder to maintain their collection. The number of prints varied each year, and it is interesting to note that none were published during the long years of WWII.
According to JTH Connor, a total of eighty three portraits were published. These show medical scenes that range from prehistory, trough Egypt, Greece, Rome, the Middle Ages, the Renaissance, all the way to the 19th century. The list of individuals portrayed is itself worth of research, as all of them in one way or another influenced medicine and surgery. Albucasis, Avicenna, Celsus, Fallopius, Fabricius, Galen, Harvey, Hunter, Rhazes, and Vesalius are but some of the tableaux vivants created for D&G.
Hillier was criticized for the lack of accuracy in some of the portraits as well as the person depicted, but the ideas for the topics were not his. The consultant used by D&G to suggest the topics was Samuel Harvey (1886-1953), who himself studied under the tutelage of famous neurosurgeon and medical historian Harvey Cushing (1869-1939).
Some of the images were later published in a book by Hillier (“Surgery through the ages”, 1944) showing other tableaux made for other medical publications.
This article continues here: The interesting story of “Sutures in Ancient Surgery (2)"
- Details
This article is part of the series "A Moment in History" where we honor those who have contributed to the growth of medical knowledge in the areas of anatomy, medicine, surgery, and medical research.

Folder of "Sutures in Ancient Surgery"
This article is the continuation of The interesting story of “Sutures in Ancient Surgery” (1).
3. The content of the publication, images, and controversy
Each tableaux vivant depicted a scene of history of surgery, with a short description of the individual and their accomplishments. In general, these descriptions are accurate, but very short. The objective was to allow the doctor to read the text, admire the image and leave time for the medical representative to deliver their presentation of a particular product.
Each page was printed in black and white, on a high quality paper measuring 12 by 9 ¼ inches. The paper itself was originally lightly yellowed to denote that this was an historical image. In fact, many doctors believed that these were reproductions of antique paintings, which they were not! The image itself was 6 ½ by 5 ¼ inches.
In some images it is clear that the background was painted. In fact, the image of Hyeronimus Fabricius Ab Aquapendente (157-1619) published in 1927, shamelessly copies part of the background of the 1555 title page of the Fabrica of Andreas Vesalius (1514-1564), or one of the many plagiarisms of the same book.
The controversy today lies with a number of women depicted with their nude breasts. In one case, (“Aspasia”, published in 1933) the photograph depicts five women including Aspasia, all of them showing a naked breast. Although “Sutures in Ancient Surgery” is criticized for this easy depiction of nudity, only 30% fall in this category.
Adding Aspasia of Miletus to this collection of physicians also brought criticism, not only for the nudity, but for the fact that Aspasia is a legendary figure whose life is in question as well as her place in Greek society. Some say that she was a prostitute and the regent of a house of ill repute, other say that she was a teacher of philosophy along with Socrates and that she was married to Pericles. Others say that she never existed, yet her name and life has been used in a novelized two-tome book. Why was she selected for this collection? No one knows.
Following are some images from "Sutures in Ancient Surgery".
4. Missing prints
Because these prints were presented as loose-leaf items to the doctors, many of them have been lost. Some historians comment that doctors would frame these images and use them in their offices, so a complete collection of the 83 photographs is extremely difficult to find. In once case, it is known that a hospital had the complete collection framed in one of its hallways (Sobieszek, 1988) which hospital, or what happened to that collection is unknown.
Today, the “Sutures in Ancient Surgery” folders found for sale in antique libraries have a varying number of prints, all of them incomplete. Some universities list them in their libraries and in one case, they have only three prints in their collection!
My research has been able to find the names of 76 of the tableaux vivants in this collection, but I have not been able to find the names of seven of these prints.
The folder that I received from Jack Kennedy contains 75 prints, and I am looking for the last eight including that of Teodorico Borgognoni, year of printing unknown.
If you have any or know of someone that owns a few in this collection, please contact me. I prepared an PDF file with the prints I have as well as those I do not. You can download it here.
Once again, thanks to Jack Kennedy for his addition to my collection. It has been an interesting research and I look forward to the next one!!
Sources:
1. UConn library Archives and Special Collections: Davis and Geck company records.
2. SNAC-Social Network and Archival Context: Davis and Geck Company.
3. “Soak it up: Examining bioabsorbable polymers in healthcare” Medical Plastic News
4. “The striking social tableaux vivants of Lejaren à Hillier” J.T.H. Connor. Hetkoen International
5. “Photography view; when tableaux vivants flowered in the magazines” Gene Thorton. The New York Times. March 2, 1986.
6.” Tableaux Vivants: A Long History of Recreating Art” Karolina Dzimira-Zarzycka. Daily Art May 1, 2020
7. “Medical History’s Moment in Art Photography (1920 to 1950): How Lejaren à Hillier and Valentino Sarra Created a Fashion for Scenes of Early Surgery” Journal of the History of Medicine and Allied Sciences, Volume 72, Issue 4, October 2017, Pages 381–421
8. “Aspasia” Wiki,org
9. “The Art of Persuasion: A History of Advertising Photography” Sobieszek, Robert A. 1988
10. “Aspasia” A Romance of Art and Love in Ancient Hellas” Mary J Safford German) Robert Hamerling (Translator) 1882. NY. W.S. Gottsberger, Publisher.
11. “Lejaren A. Hillier Photography Collection” University of Texas, Harry Ramson Center.
- Details
One of the most collectible books in medical sciences and specifically in human anatomy is “De Humani Corporis Fabrica; Libri Septem” (Seven books on the structure of the Human Body) published in 1543 by Andreas Vesalius. This book is known as the “Fabrica” among Vesaliana enthusiasts.
The story of the Fabrica is complicated and the books, research papers, paintings, statues, medals, etc. on Vesalius and the Fabrica number in the thousands.
The first edition of the Fabrica was published in 1543, it was well received and was followed by the second edition in 1555. Vesalius died in 1564 and no further editions of the Fabrica were published. There are several translations in different languages, the latest is the “New Fabrica” published in 2013. This book included annotations by Vesalius himself found in a 1555 Fabrica. This particular “Annotated Fabrica” has a history worth reading and is one of the most expensive books ever sold at an auction in February 2024 for 2.23 million US dollars.
Part of book collectibles are single pages cut off a book. This method was quite common among antiquarians in the late 1800’s and early 1900’s. As a book collector, I think it is not a good idea to destroy a great book in the quest to obtain more money selling it as individual pages.
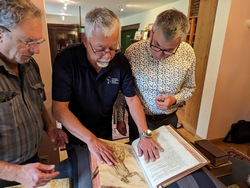
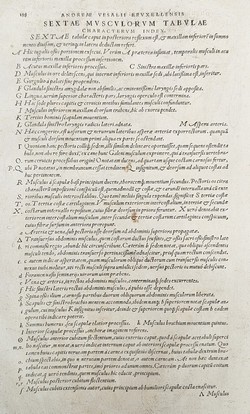
Be that as it may, in early 2023 I was notified by my good friend Dr. Randall Wolf, one of the contributors of Clinical Anatomy Associates, of an auction by Potter and Potter where two loose pages of the 1543 Fabrica would be placed on the auction block. With his help and lots of luck, I was able to secure item 298, which was a single page of the Fabrica, page 187, one of the “muscle men”, which depicts the “Liber II, Sexta Musculorum Tabula” (Book 2, Sixth Muscle Image).
One of the problems that collectors face is to prove that a certain item is original, the second one is provenance (where does the item come from?).
The first question was answered in Belgium when Dr. Wolf and I visited Dr. Francis Van Glabbeek and his personal collection in June 2023 with occasion of the 2023 Vesalius Triennial Meeting in the city of Antwerp. We were able to compare in minute detail the original image and my single page, including the type of paper and the text on the opposite page. They were a perfect match, proving that this page was indeed taken of an original 1543 Fabrica.
The second question was answered by the auctioneer, as the page belonged to the library of Ronald K. Siegel, PH.D. (1943-2019), an American psychopharmacologist and associate research professor in the Department of Psychiatry and Behavioral Sciences at the University of California, Los Angeles (UCLA). Before Dr. Siegel, we do not know how or when he acquired this single leaf of the Fabrica.
The page was carefully framed by Becky Gebhart, owner of “Picture This” in Lebanon, OH, and is secured with museum-quality glass. It in now on the wall facing my desk. Here it is:
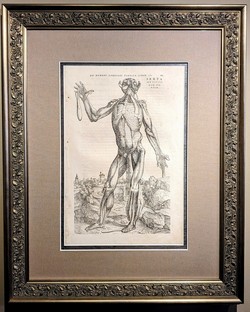 Page 188, the verso of page 187 is not visible because of the frame. This page title is "Sextæ Musculorum tabulæ charactermum index" and lists the symbols on the image.
Page 188, the verso of page 187 is not visible because of the frame. This page title is "Sextæ Musculorum tabulæ charactermum index" and lists the symbols on the image.