Medical Terminology Daily (MTD) is a blog sponsored by Clinical Anatomy Associates, Inc. as a service to the medical community. We post anatomical, medical or surgical terms, their meaning and usage, as well as biographical notes on anatomists, surgeons, and researchers through the ages. Be warned that some of the images used depict human anatomical specimens.
You are welcome to submit questions and suggestions using our "Contact Us" form. The information on this blog follows the terms on our "Privacy and Security Statement" and cannot be construed as medical guidance or instructions for treatment.
We have 3380 guests and no members online

Jean George Bachmann
(1877 – 1959)
French physician–physiologist whose experimental work in the early twentieth century provided the first clear functional description of a preferential interatrial conduction pathway. This structure, eponymically named “Bachmann’s bundle”, plays a central role in normal atrial activation and in the pathophysiology of interatrial block and atrial arrhythmias.
As a young man, Bachmann served as a merchant sailor, crossing the Atlantic multiple times. He emigrated to the United States in 1902 and earned his medical degree at the top of his class from Jefferson Medical College in Philadelphia in 1907. He stayed at this Medical College as a demonstrator and physiologist. In 1910, he joined Emory University in Atlanta. Between 1917 -1918 he served as a medical officer in the US Army. He retired from Emory in 1947 and continued his private medical practice until his death in 1959.
On the personal side, Bachmann was a man of many talents: a polyglot, he was fluent in German, French, Spanish and English. He was a chef in his own right and occasionally worked as a chef in international hotels. In fact, he paid his tuition at Jefferson Medical College, working both as a chef and as a language tutor.
The intrinsic cardiac conduction system was a major focus of cardiovascular research in the late nineteenth and early twentieth centuries. The atrioventricular (AV) node was discovered and described by Sunao Tawara and Karl Albert Aschoff in 1906, and the sinoatrial node by Arthur Keith and Martin Flack in 1907.
While the connections that distribute the electrical impulse from the AV node to the ventricles were known through the works of Wilhelm His Jr, in 1893 and Jan Evangelista Purkinje in 1839, the mechanism by which electrical impulses spread between the atria remained uncertain.
In 1916 Bachmann published a paper titled “The Inter-Auricular Time Interval” in the American Journal of Physiology. Bachmann measured activation times between the right and left atria and demonstrated that interruption of a distinct anterior interatrial muscular band resulted in delayed left atrial activation. He concluded that this band constituted the principal route for rapid interatrial conduction.
Subsequent anatomical and electrophysiological studies confirmed the importance of the structure described by Bachmann, which came to bear his name. Bachmann’s bundle is now recognized as a key determinant of atrial activation patterns, and its dysfunction is associated with interatrial block, atrial fibrillation, and abnormal P-wave morphology. His work remains foundational in both basic cardiac anatomy and clinical electrophysiology.
Sources and references
1. Bachmann G. “The inter-auricular time interval”. Am J Physiol. 1916;41:309–320.
2. Hurst JW. “Profiles in Cardiology: Jean George Bachmann (1877–1959)”. Clin Cardiol. 1987;10:185–187.
3. Lemery R, Guiraudon G, Veinot JP. “Anatomic description of Bachmann’s bundle and its relation to the atrial septum”. Am J Cardiol. 2003;91:148–152.
4. "Remembering the canonical discoverers of the core components of the mammalian cardiac conduction system: Keith and Flack, Aschoff and Tawara, His, and Purkinje" Icilio Cavero and Henry Holzgrefe Advances in Physiology Education 2022 46:4, 549-579.
5. Knol WG, de Vos CB, Crijns HJGM, et al. “The Bachmann bundle and interatrial conduction” Heart Rhythm. 2019;16:127–133.
6. “Iatrogenic biatrial flutter. The role of the Bachmann’s bundle” Constán E.; García F., Linde, A.. Complejo Hospitalario de Jaén, Jaén. Spain
7. Keith A, Flack M. The form and nature of the muscular connections between the primary divisions of the vertebrate heart. J Anat Physiol 41: 172–189, 1907.
"Clinical Anatomy Associates, Inc., and the contributors of "Medical Terminology Daily" wish to thank all individuals who donate their bodies and tissues for the advancement of education and research”.
Click here for more information
- Details
- Written by: Prof. C. Uribe

The anatomical framework of the seven books
that comprise Vesalius' Fabrica
As an educator with over 20 years teaching Human Anatomy, I have witnessed how accurate and up-to-date language can transform teaching and learning in health sciences.
The recent publication of Anatomical Terminology 2 (TA2), made freely available by the International Federation of Anatomists' Associations (IFAA), represents a significant advance that all professionals in the field should adopt as soon as possible.
Anatomical terminology is not simply a list of terms, but the basis for clear, effective and universal communication. The TA2 update addresses not only necessary changes resulting from new anatomical research and discoveries, but also substantial improvements in consistency and accuracy. This is especially relevant today, when globalization and digitalization demand accurate communication between professionals from different countries and specialties.
Using TA2 involves:
- Unifying anatomical criteria globally.
- Facilitating the teaching of anatomy with clear and precise terms.
- Improving the quality and safety of healthcare by reducing misunderstandings.
- Empowering scientific research by ensuring consistency in academic publications.
I invite fellow teachers, students and health professionals to familiarize themselves with TA2 and actively apply it in their academic and clinical practices. Let us take advantage of this tool to continue raising the standard of our work and the quality of anatomy education.
You can consult TA2 directly at this link: https://libraries.dal.ca/Fipat/ta2.html
What has been your experience with the update of anatomical terminologies?... Are you ready to integrate TA2 into your teaching and professional practice?
- Details
- Written by: Efrain A. Miranda, Ph.D.
Recientemente recibí un libro de Chile. Este libro está en Francés y se titula “Traité D’Accouchements” (Tratado sobre el Parto) o “Tratado de Obstetricia”, y se publicó en 1898 en París. El autor es el Dr. Pierre-Victor Alfred Auvard (1844 - 1940), un Ginecólogo-obstetra Francés,
El libro pertenecía a la biblioteca del Hospital San José. El Antiguo Hospital San José es un exhospital ubicado en la calle San José, a un costado del Cementerio General de Santiago, en la comuna de Independencia, ciudad de Santiago, Chile. Construido entre los años 1841 y 1872 funcionó como hospital hasta 1999, cuando se construyó el nuevo Hospital San José.Este hospital ahora está siendo demolido y se construirá uno nuevo en su lugar, pero los libros viejos de la biblioteca fueron desechados sin contemplaciones.Un ingeniero a cargo de las nuevas obras logró rescatar algunos de estos libros y uno de ellos fue traído de Chile a Estados Unidos por otro amigo mío, Carlos Verdugo, compañero de colegio.
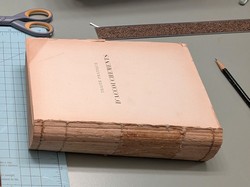
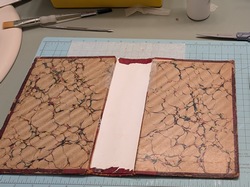
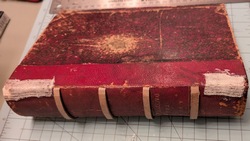
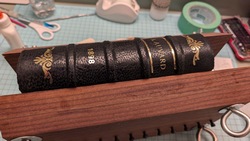
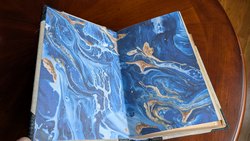
El libro estaba en pésimas condiciones, con un título apenas legible, el lomo roto y los folletos internos separados porque los hilos que lo sujetaban estaban rotos. Como la encuadernación y la reparación de libros son otra de mis aficiones, me encargué de la tarea y ahora se añadirá a mi colección. Aquí hay algunas fotos del proceso. Haga clic en la imagen para verla más grande.
En una de sus páginas, el libro tiene un sello antiguo y apenas legible que dice "Manuel Casanueva del C". Una breve búsqueda indicó que se trataba del sello Ex-Libris del cirujano chileno Dr. Manuel Casanueva del Canto. Por supuesto, tuve que investigar un poco sobre el antiguo propietario de este libro.
Manuel Casanueva del Canto nació en la ciudad de Linares, Chile, el 5 de julio de 1908. De 1925 a 1931 cursó del primero al sexto año de medicina en la Facultad de Medicina de la Universidad de Chile (donde yo estudié). En ese entonces, la Facultad de Medicina estaba en el barrio Independencia de Santiago. En 1930 obtuvo su licenciatura en medicina.

El libro reparado en mi biblioteca
Entre 1930 y 1931 fue residente de cirugía en el Hospital San Francisco de Borja (donde fue paciente de niño), pasando por Medicina Interna, Medicina de Urgencias y Cirugía y Obstetricia, obteniendo su título de cirujano en mayo de 1932. Su tesis de grado se tituló “Anatomía Patológica: Alteraciones inflamatorias de la vesícula biliar”.
Como cirujano, trabajó en el Hospital Militar de Santiago, el Servicio Central de Urgencias y el Hospital Central de Traumatología. En 1952, volviendo a sus orígenes, se trasladó al Departamento de Cirugía de la Universidad de Chile, en el Hospital José Joaquín Aguirre. Este hospital se encuentra en el mismo campus que la Facultad de Medicina donde estudió.
En 1955 postuló (y obtuvo) el puesto de Profesor Extraordinario de Cirugía Patológica en la Facultad de Medicina de la Universidad de Chile. Para entonces, ya contaba con una destacada trayectoria docente, varios premios médicos, y fue autor del libro "Transfusión Sanguínea Práctica" en 1939, además de ser coautor de varios libros médicos y más de 81 artículos.
Se convirtió en Jefe de Cirugía del Hospital José Joaquín Aguirre y en 1961 invitó a Pablo Neruda, chileno ganador del Premio Nobel de Literatura, a impartir una conferencia en el hospital.
En 1975, la Editorial Andrés Bello publicó su libro "Cirugía", en dos volúmenes en español. No he podido encontrar este libro. No se sabe mucho de él después de esta fecha. No se ha encontrado ninguna fotografía ni retrato.
Se casó con María Yolanda Carrasco Coral (fecha desconocida) y tuvieron tres hijos: María Cristina, Isabel y Manuel Luis.
Falleció el 13 de febrero de 1981 en Viña del Mar y está enterrado en Santiago de Chile. Investigaciones posteriores indicaron que este libro que recibí de regalo fue donado a la biblioteca del Hospital San José por el Dr. Casanueva, donde finalmente fue desechado, rescatado, transportado a Estados Unidos y reparado.
Espero que este artículo llegue a la los descendientes de la familia Casanueva del Canto en Linares (hoy son Casanueva Carrasco y/o Casanueva Iommi) y que me ayuden a actualizar esta investigación y tal vez obtener una foto del Dr. Casanueva del Canto. El artículo original en Inglés puede leerse aquí.
- Details
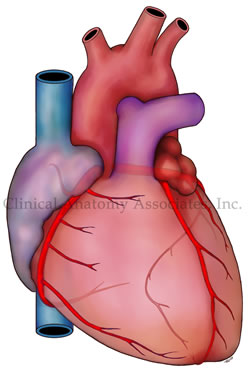
Personal Note: A few weeks ago, I came across a very interesting article in Spanish by Dr. Jose Manuel Revuelta from the University of Cantabria, Spain. The article (in Spanish) talked about the “small brain inside the heart”. One of my interests in the anatomy of the heart is the intrinsic system called the cardiac “ganglionated plexuses”, “ganglionated plexi”, or “GPs”.
It is our proposal that this nervous system inside the heart, which works autonomously (if needed to or forced to) and also dependent, of the autonomic nervous system, is responsible for the intrinsic working of the heart and its dysfunction is probably the root of cardiac dysrhythmias. We have several seminars on this topic here.
In a recent publication with Dr. Randall K. Wolf, we explained both the Wolf Procedure and the anatomical basis that underline atrial fibrillation.
The concept of the "small brain of the heart" is not new. It has been mentioned by Woolard (1926), Armour (1997), Pauza (2000), and others. These authors and others are referenced in this publication. Unfortunately, the diffusion of the concept of an intrinsic, interconnected mesh of clusters of neurons within the heart and other organs that have rhythmic activity, has many names used by the media. That is why you can find articles on the "little brain of the gut", the "gut brain", the "enteric nervous system", the "little brain of the heart", etc.
Dr. Revuelta's article shows that the interest on the GPs continues on, and more research is being done on this topic. He has graciously granted us permission to translate and publish his article in “Medical Terminology Daily”. He has also expressed interest in publishing some of his articles in this blog. Dr. Miranda
The “Little Brain” Inside the Heart
Dr. José Manuel Revuelta Soba
Professor of Surgery. Professor Emeritus, University of Cantabria, Spain
In December 2024, the prestigious journal Nature Communications published that a group of researchers from the Karolinska Institute (Sweden) and Columbia University (United States) have discovered that the heart contains a small autonomous brain.
In general, scientific knowledge has been relating cardiac activity to the brain, as the only organ that regulates its functioning. This intimate bidirectional relationship regulates the adaptation of its rhythm and contractile force to changing energy demands, through impulses and signals transmitted by the autonomic nervous system. However, the heart surprises us again with new properties that go beyond what is known.
Autonomic nervous system
The neurovegetative nervous system of the human being is involuntary, comprising the sympathetic and parasympathetic nervous systems, essential for the functioning of the organism. They act in conjunction with the enteric nervous system, which also has involuntary action and regulates the activity of the gastrointestinal tract. The complex interactions between these autonomous systems, which have opposing actions, maintain cardiovascular homeostasis, that is, they provide the appropriate amount of oxygenated blood to the organs and tissues according to their demands.
The sympathetic nervous system regulates, among other functions, the body's response to any danger perceived as a threat to physical or mental health, known as the "fight or flight" reaction, described in 1915 by the physiologist Walter B. Cannon in the United States. This instinctive reaction leads to the immediate release of certain chemical substances into the blood, such as adrenaline and noradrenaline. These hormones act as neurotransmitters that produce an increase in the contractile force of the heart, tachycardia, contraction of blood vessels, hypertension and dilation of the airways. These neurotransmitters are released in the brain, facilitating the diffusion of their messages through the extensive network that forms this autonomous nervous system, increasing the state of alertness and eliminating any feeling of drowsiness. By producing an immediate tachycardia, it improves the supply of oxygen to the organs and tissues, enlarges the pupils and reduces the digestion of food to save energy and make it available for this reaction to an unexpected danger.
The parasympathetic nervous system controls the relaxation of the body at the end of the stress caused by the sudden “fight or flight” reaction, once the threat has passed, restoring the normal functioning of the organism. Its main function is the conservation and storage of energy through the release of acetylcholine, a powerful neurotransmitter, discovered by the English physiologist Henry H. Dale, for which he was awarded the Nobel Prize in Medicine in 1936. This substance produces vasodilation, reduction of blood pressure, decreased heart rate and increased intestinal motility.
The enteric nervous system has the exclusive mission of regulating the functioning of the gastrointestinal tract, which is completely covered by hundreds of millions of nerve fibers that transmit brain messages for digestive mobility and function, modifying the volume of blood flow via vasoconstriction or vasodilation.
The small brain of the heart
The innervation of the heart is more complex than previously thought, conditioned by messages from the autonomic nervous system and others from the organ itself. In the early 1990s, scientists described that the heart contained some neurons similar to those in the human brain, which led to speculation about the possible existence of independent neuronal activity within the heart that mediated its functioning and rhythm. This fascinating discovery soon became a priority objective of scientific research.
In 2021, James S. Schwaber and R. Vadigepalli, researchers at Thomas Jefferson University in Philadelphia, performed a three-dimensional mapping of the heart's neural center. They found that the heart receives constant information from the brain about the internal and external state of its environment, adjusting heart rate, blood pressure, and cardiac output. However, these messages also came from the heart's own neural system, called the "little brain," behaving as if there were an internal loop, something similar to what systems engineers call a programmable logic controller or PLC. Most of these neurons are located near the aortic and pulmonary valves, with their largest neuronal cluster (74 percent) located in the area of the sinoatrial plexus, on the upper lateral wall of the right atrium, in immediate relation to the mouth of the superior vena cava.
Using mathematical models, they observed that when this peculiar neural programmable logic controller was activated, it perfectly adjusted the heart's response to the various impulses and signals from the brain to improve cardiac performance, making its work more efficient. Without the presence of this "little brain" it would be impossible to eliminate or correct the possible errors and damage contained in some brain messages, so the heart could become erratic, causing irregular heartbeats or arrhythmias, as well as defects in its contractility.
As these scientists analyze their 3D heart models, obtained from various mammals, new questions arise about the actions of this "brain of the heart", its internal organization, its influence on the contractile force and rhythm of the heart, as well as its coordination and responses to the constant messages from the brain. Currently, these three-dimensional maps are being used to better understand how the vagus nerve connects with cardiac neurons, opening new opportunities for the greater integration of systems engineering into the field of cardiology.
Recent findings from the Karolinska Institutet and Columbia University have revealed that the heart does indeed have its own “mini-brain,” containing a nervous system that self-regulates its rhythm and function according to demand. This complex neurological center is made up of various types of neurons with different functions, some of which function as cardiac pacemakers.
This important research project was carried out in the zebrafish, an animal model that has great similarities with the human heart, both in terms of its heart rate and its general functioning. These scientists mapped the composition, organization and functions of neurons within this small intracardiac brain, using a combination of anatomical methods, electrophysiological techniques and neuronal RNA sequencing. They carried out a complete molecular and functional classification of intracardiac neurons, revealing a complex neuronal diversity within the heart itself.
This intracardiac neurological center is not part of the autonomic nervous system governed by the brain, contrary to what was believed. The data obtained in this interesting scientific investigation show that this “small brain” is made up of several types of independent sensory neurons with clear neurochemical and functional diversity. This population of neuronal cells allows the expression of various genes that encode various neurotransmitter receptors (glycine, glutamate, adrenergic, inotropic, GABA, muscarinic, serotonergic receptors, etc.), suggesting a complex network of neurotransmission specific to the heart, which ignores its total dependence on central orders from the brain.
“We were surprised to see the complexity of this small brain inside the heart, which has a key role in maintaining and controlling the heartbeat, similar to how the brain regulates other rhythmic functions such as locomotion and breathing. Better understanding this nervous system could lead to new insights into heart disease and help develop new treatments, such as for arrhythmias. We will continue to investigate how the heart’s brain interacts with the real brain to regulate cardiac functions under different conditions, such as exercise, stress or disease”, explains Konstantinos Ampatzis, a senior researcher at the Department of Neuroscience at Karolinska Institutet, Sweden, who led the study.
Future electrophysiological, pharmacological and molecular research will be critical to better understand the tangled interactions and complex regulatory mechanisms of the internal neurotransmission of this autonomous “small brain” and thus understand its overall regulation of cardiac rhythm, contraction and output in the face of the multiple physical and mental changes to which we are exposed throughout life.
“There is a wisdom of the head and a wisdom of the heart"
Charles Dickens (1812-1870), English writer
“Facts do not cease to exist because they are ignored”
Aldous Huxley (1894-1963), English writer and philosopher.
Sources:
1. “Decoding the molecular, cellular, and functional heterogeneity of zebrafish intracardiac nervous system”. Pedroni, A; Yilmaz, E; Del Vecchio,L; et al. Nature Communications, 2024; 15 (1) DOI: 10.1038/s41467-024-54830-w
2. Bodily changes in pain, hunger, fear, and rage; an account of recent researches into the function of emotional excitement” Cannon, W. 1915. D. Appleton and Co. USA.
3. “Mapping the little brain at the heart by an interdisciplinary systems biology team” Vadigepalli, Rajanikanth et al. iScience, Volume 24, Issue 5, 102433. https://doi.org/10.1016/j.isci.2021.102433
4. A comprehensive integrated anatomical and molecular atlas of rat intrinsic cardiac nervous system. Achanta S. et al. iScience 2020 Jun 26;23(6):101140 doi: 10.1016/j.isci.2020.101140
5. "Minimally Invasive Surgical Treatment of Atrial Fibrillation: A New Look at an Old Problem" Randall K. Wolf, Efrain A. Miranda, Operative Techniques in Thoracic and Cardiovascular Surgery, 2024, doi.org/10.1053/j.optechstcvs.2024.10.003
6 Valenza, G., Matić, Z. & Catrambone, V. The brain–heart axis: integrative cooperation of neural, mechanical and biochemical pathways. Nat Rev Cardiol 22, 537–550 (2025).
- Details
On January 23rd, 2025, I was invited to deliver a lecture on “Human Anatomical Models: History and Development of Plastination”. The lecture was delivered at the Anatomy Learning Lab which is found at the Donald C. Harrison Health Sciences Library at the University of Cincinnati.
As you may know, I am quite interested in the history of Medical Sciences and one of the topics is the history of surgical stapling. I have written extensively on this topic, including chapters in books, and the life and works of Dr. Mark M. Ravitch.
At this lecture among the attendees were several colleagues and friends and one special guest, the great granddaughter of Dr. Ravitch. Her name is Mila Colizza and she is a first year medical student here at the University of Cincinnati.
Keeping the medical tradition of the Ravitch family… Way to go Mila!!!. My best wishes in your medical career.
- Details
This article is part of the series "A Moment in History" where we honor those who have contributed to the growth of medical knowledge in the areas of anatomy, medicine, surgery, and medical research.
Leon C. Hirsch (1927 – 2023). The story of the development of surgical staplers in America cannot be told without the presence and vision of Leon Hirsch, an American business executive and entrepreneur...
After his 1958 trip to the USSR with two other surgeons, Dr. Mark Ravitch tried to have his colleagues take interest in the surgical stapling technology. Dr. Ravitch and Dr. Felicien Steichen stated in one of their books “Interestingly enough, a number of American manufacturers, knowing of our interest, visited our laboratories and operating rooms to see how the staplers performed, but for one reason or another decided that there was no future in stapling – to their later expressed regret! (1)”
There have been several apocryphal stories, including one where L. Hirsch was a down-on-his luck shoe salesman (not true) that met with his friend Ravitch as they both lived close to each other (not true either). So, what is the real story of how Leon Hirsch met Mark Ravitch and founded the United States Surgical Corporation (USSC).?
The original story, as told by Leon Hirsch, can be found in the May 1990 edition of the medical journal “Surgical Rounds” (2), an edition entirely dedicated as a “Festschrift (commemorative publication) to Mark Ravitch, MD”, after his death.
Leon Hirsch says: “In 1963, I was engaged in a discussion with a patent broker in New York City when I noticed a strange-looking metal object on his desk, which he described to be a Russian surgical stapler. Further inquiry led to the disclosure that this patent broker had been retained by the Russian government to try to market Soviet-made surgical staplers in America”. This patent broker had tried to garner the attention of at least five companies (Ethicon, Davis & Geck, American Hospital Supply, Aloe Corp., and Ipco, Inc) with no success.
This statement by Leon Hirsch goes against everything I knew, that is, that Dr. Ravitch was the one trying to bring the patents from the then USSR to the USA. In another version of this story Dr. Ravitch bought the patents and tried to sell them to USA medical companies! None of these are true.
Leon Hirsch continues “The patent broker offered to lend me his information book on Russian stapling… the package disclosed that recently, three American surgeons had been to Moscow to study Russian surgical techniques, including the technique of surgical stapling”. This statement by the Soviet government is not correct, as Dr. Ravitch and two other surgeons had been to Moscow, yes, but to study Russian transfusion and resuscitation techniques, and the fact that they ended observing surgery (and seeing surgical staplers at work) was serendipitous. That in itself is another story.
Leon Hirsch phoned Dr. Ravitch who at the time was working at John Hopkins. They planned to meet for 15 minutes, which stretched into lunch, then back to Dr. Ravitch’s office for a demo of the staplers. The discussion veered into the difficulty of loading the staples one by one in this large, cumbersome device. “Intrigued, I asked Dr. Ravitch to borrow the instrument, took it back to my home workshop, and realized that the answer to the loading problem was to separate the instrument from the staples. I made a model of a cartridge (in balsa wood) that could be preloaded with staples and easily slipped into the instrument. Dr. Ravitch was elated”. The idea of the interchangeable cartridge was Hirsch's!
With this idea, and financial support that he pursued, Leon Hirsch proceeded to form the United States Surgical Corporation, with four initial employees. It took three years (1964-1967) to develop a stainless steel surgical stapler that had interchangeable preloaded stapler cartridges that were up to American standards. Since then, thousands of patients have benefited from these devices.
An interesting side note is that Leon Hirsch wanted Mark Ravitch to play a part in this new company, but Ravitch declined. Hirsch states: "Dr. Ravitch said that he had no commercial interest in pursuing such a project but he would be willing and happy tp evaluate, first in the laboratory and if successful clinically, such new devices. In typical Ravitch fashion he added that he planned to report exactly what he found, good or bad".
The story of USSC continued through acquisitions, so USSC became Tyco, then Tyco Healthcare, Covidien, and today is the Stapling Division of Medtronic.
Leon Hirsch and USSC confronted the conundrum of training surgeons in the use of the new staplers. To this end he initially hired eight nurses, but eventually created a six-week extremely difficult grueling training program that took sales representative from basic medical terminology to being able to direct the surgeon through the steps on the use of the surgical staplers in the procedure. By doing this, he changed the way medical devices surgical representatives operate in the medical arena. Some of the readers of this article probably went through this challenging training program! In fact, some medical companies started trying to hire people that had been trough this training.
Drs. Ravitch and Steichen continued their quest training surgeons on the benefits of surgical stapling, while at the same time testing and improving the newer devices that Leon Hirsch and USSC developed.
In 2018, The Mullings Group interviewed Leon Hirsch (then 91 years old) and published a video of this interview, where he covers these topics and more. This video now forms part of the History of Surgical Stapling.
My personal thanks to Joe Mullings, Chairman & CEO of the Mullings Group Companies for his permission to share this video and some video captures for this article.
Sources:
1. “Current Practice of Surgical Stapling” Ravitch, M; Steichen, F; Welter, R. 1991 Lea & Febiger Publishers, USA.
2. “Festschrift to Mark Ravitch, MD” Surg Rounds J. May 1990. Romaine Pierson Publication.
3. "Stapling in Surgery" Ravitch, MM; Steichen, FM.1984 Yearbook Medical Publishers USA.
4. The Origin of Medical Terms" Skinner 1970
5. "Notes by Dr. Mark Ravitch on Trip to Russia - September 1958" Personal notes.
6.“Leon Hirsch: Opportunity is Everywhere” YouTube video by the Mullings Group. Oct 2018
7. “Tribute to Felicien Steichen” SAGES Minimally Invasive Surgery Videos. April 2012
All images are in the public domain, or. have been authorized for use.
- Details
This article is part of the series "A Moment in History" where we honor those who have contributed to the growth of medical knowledge in the areas of anatomy, medicine, surgery, and medical research.
Young surgeons today use surgical staplers without a thought as to the history of the development of these surgical devices. The same is true for many who work in the medical devices (surgical staplers) industry. I have worked as a consultant and a trainer for the stapler industry both with Ethicon Endosurgery (today Ethicon, stapling division) and the United States Surgical Corporation (today Medtronic, stapling division) and developed a special interest in the medical history related to the origin, research, and development of surgical staplers.
The history of surgical stapling is quite interesting and has many characters, starting with the early works of Humer Hutl. There are whole books dedicated to this topic.
It cannot be denied that one of the main drivers of surgical stapling in the United States was Dr. Mark M. Ravitch (1910-1989). History tells us that he saw these staplers in action being used by Dr. Nikolai Mikhailovich Amosov (1913–2002) during a visit to the Thoracic Surgical Institute in Kiev in September 1958. Kiev was then part of Russia (then called the USSR).
What I did not know is that Dr. Ravitch had his notes typewritten, and those loose leaf notes are now part of my library in a binder.
The notes in this binder are the carbon copies in onionskin paper of notes typewritten personally by Dr. Mark. M. Ravitch during his trip to the USSR in September 1958. According to his family, Dr, Ravitch had notoriously bad handwriting and he liked to maintain records of his work, so he was a very fast typewriter. He used his personal typewriter and he traveled everywhere with it even during his military service in WWII.
The original notes were bound in a book (also in my collection) and gifted by Dr. Ravitch to his parents. Unfortunately, the paper he used for the originals was not acid-free and the pages in this unique book are slowly crumbling and some of them are today unreadable. Thankfully, the carbon copies are acid-free, and the pages have been carefully scanned in TIF and PDF format by David M. Klein and then placed in separate plastic sleeves for preservation in a binder that is now in my library.
After Dr. Ravitch’s parents passing, both these notes were in the library of his son, Michael M. Ravitch, Ph.D. Michael lent these notes to Dr. Felicien Steichen (1926 – 2011) , who after a time returned the notes with a letter, also included in this binder. In this letter Dr. Steichen says that these notes should be preserved for future research, even mentioning Leon Hirsch (CEO of the United States Surgical Corporation) to support this endeavor.
Michael Ravitch’s widow, Myrnice Ravitch contacted me in 2017 because of my interest in medical history and the life and work of Dr. Ravitch. She donated some books that were in Dr. Ravitch’s library. In early 2024, and with the blessing of Dr. Ravitch’s daughter Binnie and the rest of the Ravitch family, they donated these notes that are now part of the history of surgical stapling and are today part of my library.
In a separate article I will present some of the actual notes regarding surgical stapling, although these notes also include invaluable observations on medicine and surgery in the USSR and Dr. Ravitch’s comments on the Russian culture and people at the time. Keep in mind that Dr. Ravitch’s parents where Russian immigrants and he was fluent in Russian.
In the future, and following Dr. Steichen’s suggestion, I will try to publish a book with these notes along with additional notes on Dr. Ravitch’s trip to China in 1983
Note: The photograph of Dr. Asomov was taken by Dr. Ravitch, but it has since degraded, so it was enhanced using Winxvideo AI.
Note: Dr. N.M. Amosov had an incredible surgical career and recognized with medals and honors. The Institute where Dr. Ravitch saw him operate with surgical staplers is today known as the Amosov National Institute of Cardiovascular Surgery in Kiev, Ukraine.
Sources:
1. "Current practice of surgical Stapling" Ravitch, MM; Steichen, FM; Welter,W. 1991 Lea & Ferbiger USA
2. "Stapling in Surgery" Ravitch, MM; Steichen, FM.1984 Year Book Medical Publishers USA.
3. "Surgical Rounds" Edition dedicated to Dr. M.M. Ravitch May 1990
4. "Notes by Dr. Mark Ravitch on Trip to Russia - September 1958" Personal notes, unpublished.