Medical Terminology Daily (MTD) is a blog sponsored by Clinical Anatomy Associates, Inc. as a service to the medical community. We post anatomical, medical or surgical terms, their meaning and usage, as well as biographical notes on anatomists, surgeons, and researchers through the ages. Be warned that some of the images used depict human anatomical specimens.
You are welcome to submit questions and suggestions using our "Contact Us" form. The information on this blog follows the terms on our "Privacy and Security Statement" and cannot be construed as medical guidance or instructions for treatment.
We have 833 guests and no members online

Jean George Bachmann
(1877 – 1959)
French physician–physiologist whose experimental work in the early twentieth century provided the first clear functional description of a preferential interatrial conduction pathway. This structure, eponymically named “Bachmann’s bundle”, plays a central role in normal atrial activation and in the pathophysiology of interatrial block and atrial arrhythmias.
As a young man, Bachmann served as a merchant sailor, crossing the Atlantic multiple times. He emigrated to the United States in 1902 and earned his medical degree at the top of his class from Jefferson Medical College in Philadelphia in 1907. He stayed at this Medical College as a demonstrator and physiologist. In 1910, he joined Emory University in Atlanta. Between 1917 -1918 he served as a medical officer in the US Army. He retired from Emory in 1947 and continued his private medical practice until his death in 1959.
On the personal side, Bachmann was a man of many talents: a polyglot, he was fluent in German, French, Spanish and English. He was a chef in his own right and occasionally worked as a chef in international hotels. In fact, he paid his tuition at Jefferson Medical College, working both as a chef and as a language tutor.
The intrinsic cardiac conduction system was a major focus of cardiovascular research in the late nineteenth and early twentieth centuries. The atrioventricular (AV) node was discovered and described by Sunao Tawara and Karl Albert Aschoff in 1906, and the sinoatrial node by Arthur Keith and Martin Flack in 1907.
While the connections that distribute the electrical impulse from the AV node to the ventricles were known through the works of Wilhelm His Jr, in 1893 and Jan Evangelista Purkinje in 1839, the mechanism by which electrical impulses spread between the atria remained uncertain.
In 1916 Bachmann published a paper titled “The Inter-Auricular Time Interval” in the American Journal of Physiology. Bachmann measured activation times between the right and left atria and demonstrated that interruption of a distinct anterior interatrial muscular band resulted in delayed left atrial activation. He concluded that this band constituted the principal route for rapid interatrial conduction.
Subsequent anatomical and electrophysiological studies confirmed the importance of the structure described by Bachmann, which came to bear his name. Bachmann’s bundle is now recognized as a key determinant of atrial activation patterns, and its dysfunction is associated with interatrial block, atrial fibrillation, and abnormal P-wave morphology. His work remains foundational in both basic cardiac anatomy and clinical electrophysiology.
Sources and references
1. Bachmann G. “The inter-auricular time interval”. Am J Physiol. 1916;41:309–320.
2. Hurst JW. “Profiles in Cardiology: Jean George Bachmann (1877–1959)”. Clin Cardiol. 1987;10:185–187.
3. Lemery R, Guiraudon G, Veinot JP. “Anatomic description of Bachmann’s bundle and its relation to the atrial septum”. Am J Cardiol. 2003;91:148–152.
4. "Remembering the canonical discoverers of the core components of the mammalian cardiac conduction system: Keith and Flack, Aschoff and Tawara, His, and Purkinje" Icilio Cavero and Henry Holzgrefe Advances in Physiology Education 2022 46:4, 549-579.
5. Knol WG, de Vos CB, Crijns HJGM, et al. “The Bachmann bundle and interatrial conduction” Heart Rhythm. 2019;16:127–133.
6. “Iatrogenic biatrial flutter. The role of the Bachmann’s bundle” Constán E.; García F., Linde, A.. Complejo Hospitalario de Jaén, Jaén. Spain
7. Keith A, Flack M. The form and nature of the muscular connections between the primary divisions of the vertebrate heart. J Anat Physiol 41: 172–189, 1907.
"Clinical Anatomy Associates, Inc., and the contributors of "Medical Terminology Daily" wish to thank all individuals who donate their bodies and tissues for the advancement of education and research”.
Click here for more information
- Details

Histology image of cardiac muscle*
[UPDATED] Cardiac muscle is one of the three types of muscle found in the human body. It is found exclusively in the heart, where it forms the main component of its middle layer, the myocardium.
[Myo]=combining form for "muscle"; [-card-]=heart; and [-ium]=layer or membrane. The myocardium is the muscle layer of the heart.
Cardiac muscle has distinct striations and intercalated discs (see accompanying image). The cardiac muscle acts as a functional syncytium.
The key characteristic of cardiac muscle is automatism or automaticity, its capacity to contract rhythmically in the absence of an external electrical stimulus. The other two types of muscle (smooth and skeletal) lack this characteristic.
The term [cardiomyocyte] can be used to describe each of these cells as the word is composed of [Card(i)o=combining form for "heart"; [myo]=combining form for "muscle"; and the suffix [-cyte]= cell. A cardiomyocyte is a cardiac muscle cell.
The conduction system of the heart is made exclusively of cardiomyocytes, and is part of a more complex rhythm control system of the heart.
Image modified from the original on YouTube from the British Heart Foundation.
* Original histology image by S, Girod and A. Becker, courtesy of Wikipedia.
- Details
- Written by: Efrain A. Miranda, Ph.D.
[UPDATED] These two root terms mean "heart".
The first one, [-card(i)-] arises from the Greek [καρδιά] pronounced kardiá, and can be seen in medical words such as: cardiac, echocardiogram, cineangiocardiogram, cardioplegia, myocardial infarction, etc.
The second one [-cord(i)-] arises from the Latin [cor] or [cordis] and can be seen in words such as: precordial pain, cordial, commotio cordis, etc.
As a point of interest, the original Greek spelling of [kardium] was used by Nobel prize winner Dr. Willem Einthoven (1860 - 1927) when he invented the electrocardiograph and the electrocardiogram. The German term is [elektrokardiogramm] and the German abbreviation for the procedure is EKG. Since we use the term in English, [electrocardiogram] we use the abbreviation ECG. Both are correct, although if you are speaking English, ECG should be used.
* Image property of:CAA.Inc.. Artist:Victoria G. Ratcliffe
- Details

Vine tendril. Image courtesy of Jon Sullivan
The term [pampiniform] comes from the Latin term [pampinus] meaning "a vine tendril". It refers to a twisted, curved structure as seen in the accompanying image. The second portion of the word also comes from Latin, [forma] means "shape" or "in the shape of".
Pampiniform then means "in or with the shape of a vine tendril"
Although mostly associated with the pampiniform plexuses found in both the testicular veins in the spermatic cord and the ovarian veins found within the infundibulopelvic ligament, the term is also used to denote the coiled aspect of the organ of Rosenmuller, also known as the pampiniform body or paraovarium.
The pampiniform body is a non-functional embryological remnant of the development of the female reproductive system. It is composed of a blind longitudinal duct and 10-15 transverse smaller ducts. It is located in the mesosalpinx, an extension of the broad ligament related to the uterine tube (Fallopian tube).
Thanks to David Van Tol for suggesting this article!
Image courtesy of Jon Sullivan, Public domain, via Wikimedia Commons https://jonsullivan.com/
- Details
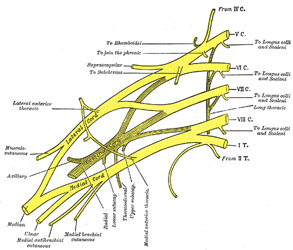
UPDATED: The term [plexus] comes from the Latin term [plectere] meaning " to twine, or to braid". In anatomy, the term [plexus] refers to a group of structures that are intertwined or form a meshwork. The plural form is [plexuses], although the Latin plural form [plexi] is also correct. Gabrielle Fallopius used the term to denote "a tangle of nerves"
There are many plexuses described in the human body. Most are formed by nerves, but there are many that are lymphatic or vascular. The best known are the plexuses of nerves formed by the ventral rami of the spinal nerves. These are the cervical plexus, the brachial plexus, the lumbar plexus, and the sacral plexus. The image depicts the brachial plexus. For a larger version, click on the image, and for further information on the cervical and brachial plexuses, click here.
Images and links courtesy of:www.bartleby.com
- Details
- Written by: Efrain A. Miranda, Ph.D.
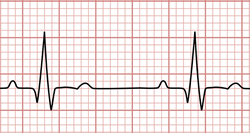
Sinus rhythm electrocardiogram
A contraction, from the Greek [διαστολη] (systolí) meaning “expansion, dilation, drawing out, or prolongation”, also [διαστέλλειν] (diastéllein) meaning “to open, expansion”. When used in music, it means "a pause".
It refers to the dilation of the heart. If you analyze a normal heartbeat (sinus rhythm), there are two diastoles: an atrial diastole and a ventricular diastole. The term diastoleis usually used in reference to the ventricular diastole.
Diastole was first recognized and named by Herophilus of Alexandria (325-255BC), most probably trough animal vivisection. Herophilus was accused of animal vivisection and the dissection of human cadavers. Because of this, some call Herophilus "The Father of Anatomy".
Galen of Pergamon (129AD - 200AD) used the term [διαστέλλεσθαι] (diastéllesthai), also meaning “expansion”.
The word in English was first used in the 16th century. The modern pronunciation in English follows the Greek pronunciation by ending the word in a long “e” as in “to be”.
Sources
1. "The Origin of Medical Terms" Skinner, HA 1970 Hafner Publishing Co.
2. "Medical Meanings - A Glossary of Word Origins" Haubrich, WD. ACP Philadelphia
3. "Dorlands's Illustrated Medical Dictionary" 26th Ed. W.B. Saunders 1994
4. "Greek anatomist Herophilus: the father of anatomy" Si-Yang, N. Anat Cell Biol. 2010; 43(4): 280–283
Note: Google Translate includes an icon that will allow you to hear the pronunciation of the word
- Details
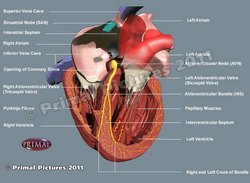
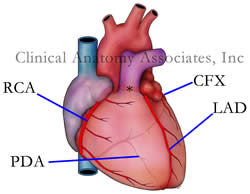
Conduction system of the heart
[UPDATED] The conduction system of the heart is part of a complex intrinsic heartbeat and rhythm control system that includes a cardiomyocyte-based component which acts as an automatic base, and an extrinsic and intrinsic autonomic nervous system component which acts as a modulator.
The classic description of the conduction system of the heart emphasizes only the cardiomyocyte-based component and refers to a group of specialized cardiac muscle structures that serve as pacemakers and distributors of the electrical stimuli that make the heart beat coordinately. It is important to stress the fact that this primary "conduction system of the heart" is not formed by nerves but rather by specialized cardiac muscle cells.
Components of the cardiomyocyte-based conduction system of the heart:
• SA node: The sinoatrial (SA) node is a small nodule of cardiac muscle tissue, somewhat horseshoe-shaped that is found at the junction of the superior vena cava and the right atrium. It receives blood supply from the SA node artery, a branch of the right coronary artery. Later research indicates that the pacemaker function of the SA node includes areas of the lateral wall of the right atrium which are involved in different heart rate speeds. It is also known eponymically as the "node of Keith and Flack" after Sir Arthur Keith (1866 - 1955) and Martin Flack, CBE (1882 - 1931).
The electrical impulses propagate between the right and left atria by way of the interatrial bundle, also known as "Bachmann's bundle", and between the SA node and the atrioventricular node by way of three internodal tracts, described by James Wenckebach, and Christen Thorel. More information on these internodal tracts here.
• AV node: The atrioventricular (AV) node is found at the junction of atria and ventricles in an area known as the "Triangle of Koch". Its function is to delay the electrical impulse passing from the atria to the ventricles by 1/10th of a second, enabling the sequential pumping action of the heart. The eponymic name for the AV node is "node of Aschoff-Tawara", and it receives its blood supply by way of the AV node artery, a branch that usually arises from the right coronary artery
• AV bundle: Also known as the "Bundle of His", this thick bundle of specialized myocardial cells is found in the interventricular septum. It divides into the right and left bundle branches
• Bundle branches: Sometimes known as the "crura" of the bundle of His, these two divisions of the AV bundle help distribute the electrical stimuli to the ventricular walls. The right bundle branch has an extension that crosses the lumen of the right ventricle, from the base of the anterior papillary muscle to the interventricular septum, forming a cord of tissue known as the "moderator band" or "septomarginal trabecula"
• Purkinje Fibers: These thin fibers are the terminal end of the conduction system of the heart and finish the distribution of the electrical stimuli to all parts of the ventricular walls
Although the structural components of the conduction system of the heart were known, it was Dr. Sunao Tawara (1873-1952) who discovered the AV node and described the connections between the components of what he called the "Reitzleitungssytem" (conduction system) of the heart.
The conduction system of the heart is part of a more complex rhythm control system of the heart. For more information click here.
Click on the image for a larger version. Image modified from the original: "3D Human Anatomy: Regional Edition DVD-ROM." Courtesy of Primal Pictures.