Medical Terminology Daily (MTD) is a blog sponsored by Clinical Anatomy Associates, Inc. as a service to the medical community. We post anatomical, medical or surgical terms, their meaning and usage, as well as biographical notes on anatomists, surgeons, and researchers through the ages. Be warned that some of the images used depict human anatomical specimens.
You are welcome to submit questions and suggestions using our "Contact Us" form. The information on this blog follows the terms on our "Privacy and Security Statement" and cannot be construed as medical guidance or instructions for treatment.
We have 1128 guests and no members online

Jean George Bachmann
(1877 – 1959)
French physician–physiologist whose experimental work in the early twentieth century provided the first clear functional description of a preferential interatrial conduction pathway. This structure, eponymically named “Bachmann’s bundle”, plays a central role in normal atrial activation and in the pathophysiology of interatrial block and atrial arrhythmias.
As a young man, Bachmann served as a merchant sailor, crossing the Atlantic multiple times. He emigrated to the United States in 1902 and earned his medical degree at the top of his class from Jefferson Medical College in Philadelphia in 1907. He stayed at this Medical College as a demonstrator and physiologist. In 1910, he joined Emory University in Atlanta. Between 1917 -1918 he served as a medical officer in the US Army. He retired from Emory in 1947 and continued his private medical practice until his death in 1959.
On the personal side, Bachmann was a man of many talents: a polyglot, he was fluent in German, French, Spanish and English. He was a chef in his own right and occasionally worked as a chef in international hotels. In fact, he paid his tuition at Jefferson Medical College, working both as a chef and as a language tutor.
The intrinsic cardiac conduction system was a major focus of cardiovascular research in the late nineteenth and early twentieth centuries. The atrioventricular (AV) node was discovered and described by Sunao Tawara and Karl Albert Aschoff in 1906, and the sinoatrial node by Arthur Keith and Martin Flack in 1907.
While the connections that distribute the electrical impulse from the AV node to the ventricles were known through the works of Wilhelm His Jr, in 1893 and Jan Evangelista Purkinje in 1839, the mechanism by which electrical impulses spread between the atria remained uncertain.
In 1916 Bachmann published a paper titled “The Inter-Auricular Time Interval” in the American Journal of Physiology. Bachmann measured activation times between the right and left atria and demonstrated that interruption of a distinct anterior interatrial muscular band resulted in delayed left atrial activation. He concluded that this band constituted the principal route for rapid interatrial conduction.
Subsequent anatomical and electrophysiological studies confirmed the importance of the structure described by Bachmann, which came to bear his name. Bachmann’s bundle is now recognized as a key determinant of atrial activation patterns, and its dysfunction is associated with interatrial block, atrial fibrillation, and abnormal P-wave morphology. His work remains foundational in both basic cardiac anatomy and clinical electrophysiology.
Sources and references
1. Bachmann G. “The inter-auricular time interval”. Am J Physiol. 1916;41:309–320.
2. Hurst JW. “Profiles in Cardiology: Jean George Bachmann (1877–1959)”. Clin Cardiol. 1987;10:185–187.
3. Lemery R, Guiraudon G, Veinot JP. “Anatomic description of Bachmann’s bundle and its relation to the atrial septum”. Am J Cardiol. 2003;91:148–152.
4. "Remembering the canonical discoverers of the core components of the mammalian cardiac conduction system: Keith and Flack, Aschoff and Tawara, His, and Purkinje" Icilio Cavero and Henry Holzgrefe Advances in Physiology Education 2022 46:4, 549-579.
5. Knol WG, de Vos CB, Crijns HJGM, et al. “The Bachmann bundle and interatrial conduction” Heart Rhythm. 2019;16:127–133.
6. “Iatrogenic biatrial flutter. The role of the Bachmann’s bundle” Constán E.; García F., Linde, A.. Complejo Hospitalario de Jaén, Jaén. Spain
7. Keith A, Flack M. The form and nature of the muscular connections between the primary divisions of the vertebrate heart. J Anat Physiol 41: 172–189, 1907.
"Clinical Anatomy Associates, Inc., and the contributors of "Medical Terminology Daily" wish to thank all individuals who donate their bodies and tissues for the advancement of education and research”.
Click here for more information
- Details
This article is part of the series "A Moment in History" where we honor those who have contributed to the growth of medical knowledge in the areas of anatomy, medicine, surgery, and medical research.
This is the continuation of the article “The Ephraim McDowell House and Museum (3)”. For the first article, click here.
The rest of the house is interesting. The kitchen is an open hearth typical of the times and beneath the operating room. Candle molds, butter churners, baking tables, iron cooking utensils, etc. The guide explained that most of the cooking work was done by slaves.
To the back of the house if a large garden. Part of it is shaped as a Maltese cross, and this is where Dr. McDowell cultivated medicinal plants and herbs for his practice and the apothecary, The garden has several monuments, one of which is the original slab that covered Dr. McDowell's tomb.
The apothecary
This "pharmacy" of the times is incredibly well-preserved, maintained and furnished. It is said that Dr. McDowell worked so much at this place that he eventually moved to the country to a second house he named "Cambiskenneth" after a famous local native american chief.
The apothecary has a basement that is off-limits to visitors, but there are photographs of the location for visitors to see.
Some of the porcelain and glass containers still have some of their contents.
Additional historic buildings
Just across from the McDowell House and Museum is the Constitution Square, a site that I would encourage you to visit. Following is an excerpt of the Danville KY website on the Constitution Square Historic Site:
"This is the birthplace of Kentucky's statehood. In 1776, Kentucky was still part of the frontier and a county of Virginia. The Wilderness Road, blazed by Daniel Boone, led pioneers through the Cumberland Gap and into Central Kentucky. Danville's prominent location on the Wilderness Road caused it to become a crossroad for early settlers, and a center of political activity.
By 1785, Danville was chosen as Kentucky's first seat of government, and a meetinghouse, courthouse and jail were built to administer the growing territory. Still bound to Virginia laws, though, several Danville citizens formed the political club that recognized the need for a convention to discuss statehood. Between 1784-1792, ten constitutional conventions took place at the courthouse of Constitution Square. In 1790, Kentucky delegates accepted Virginia's terms for separation from the state. On June 1, 1792, Kentucky became the fifteenth state in the union, and Isaac Shelby, a Revolutionary War hero, was named the first Governor of the Commonwealth."
Several original buildings and replicas are found at this site.
In closing this series of articles I can only say that this was an interesting personal and learning experience. Being able to visit The Ephraim McDowell House and Museum allowed me to envision the life of this time. To place it in perspective the year that Dr. McDowell operated on Mrs. Crawford was 1809. On the same year Abraham Lincoln was born (only 35 miles from the farm of Mrs. Crawford), James Madison was the 4th president of the United States of America (which had only 15 states and 6 territories), Napoleon occupied Vienna, and Ludwig van Beethoven had just finished writing his Fifth Symphony.
Following is a large image of the original house prior to its renovation. The image is in the public domain from a biographical book by Dr. McDowell's granddaughter Mary Young Ridenbaugh.
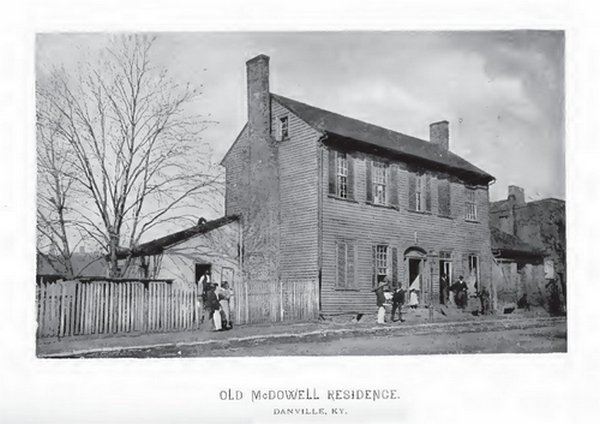
Click on the image for a larger depiction
Sources:
1. “Ephraim McDowell and Jane Todd Crawford, the Bicentennial of a Surgical Masterpiece” Benigno, BB Obst & Gynecol (2009) 113. 5:1141-1144
2. “The Biography of Ephraim McDowell, M.D.; The Father of Ovariotomy” Ridenbaugh, MY, 1890 CL Webster & Co.
3. “Ephraim McDowell: "Father of ovariotomy" and founder of abdominal surgery, with an appendix on Jane Todd Crawford” Schachner, A 1921, J.B. Lippincott Co. (Interesting discovery in an Ex-Libris in this book)
- Details
This article is part of the series "A Moment in History" where we honor those who have contributed to the growth of medical knowledge in the areas of anatomy, medicine, surgery, and medical research.
This is the continuation of the article “The Ephraim McDowell House and Museum (2)”. For the first article, click here.
The “Operating Room”
The so-called “operating room” is the place where everybody thinks a historical surgical event took place. The room is at a different level and communicates with the master bedroom. There is a plaque placed there byt Chapter XI of the Colonial Dames of America. In the room there is antique furniture and surgical instruments of the time.These are most probably not Dr. McDowell’s instruments, but I would like to believe so.
In the instrument kits you can clearly see different types of knives, lancets, needles, trephines, tourniquets, and amputation saws. What is interesting is that at the time (1809) there were no concepts of asepsia or anesthesia. So why did this historical operation did not get infected? Dr. McDowell’s habits and the location of the room may provide an answer. It is said that Dr. McDowell was very strict about bodily and environmental cleanliness (clothes and such). The location of the operating room is directly above the kitchen and has a separate set of stairs that leads directly to it. In the 1800's white linen was boiled.
In my opinion, this room was not only the “operating room” but also the “convalescent room” for people that were operated by Dr. McDowell. A room that served as pre and postoperatory, as well as an operating room.
In the room there are also additional artifacts, one of which definitely caught my attention: A doctor’s saddle bag. Since all transportation was by horse or buggy, a young doctor needed a special saddle bag that contained surgical instruments, medicine, and all that was needed for a home visit. This reminds me of a book I strongly recommend: “The horse and buggy doctor” by Arthur E. Hertzler, MD who was born almost 40 years after Dr. McDowell died.
The operation
Dr. McDowell visited Jane Todd Crawford in early December 1809 at her home 60 miles away. The reason was that two doctors wanted him to help in the birthing, as they thought the patient was pregnant and in pain. After examination Dr. McDowell explained to the patient that she had an (at the time) inoperable ovarian tumor and the she had a fatal prognosis. He also explained that he would be willing to try a risky and experimental surgery, but only at his home in Danville, KY. Mrs. Crawford agreed, as this was the only opportunity to save her life.
Mrs. Crawford, traveled very slowly for several days on horseback, crossing several rivers in the process. When she arrived she was tired and in a delicate condition, so she stayed several days before Dr. McDowell attempted the operation.
The operation itself has been described countless times. On Sunday December 25th, 1809 the patient was placed on a table in the “operating room”. Dr. James McDowell, a nephew assisted in the operation. Dr. James McDowell repeatedly asked his uncle to desist in the attempt that he was convinced was going to fail, the other physician attending was Dr. Alban Goldsmith.
The patient was given some opioids (not anesthesia), her face was covered with a light piece of cloth and while she recited psalms and sang hymns Dr. Ephraim McDowell cut a 9-inch left paramedian incision opening her abdomen. The tumor was so big that it had to be cut open initially to partially drain a “dirty, mucous content”. After a single ligature through the broad ligament and infundibulopelvic ligament, the tumor was removed. It weighed 22 and a half pounds (10.2 kgs)! The incision was closed with an interrupted suture.
Five days after the operation, when Dr, McDowell came from the master bedroom to the now “postoperative” guest room he was surprised to see Mrs. Crawford on her feet making her bed! In Dr. McDowell’s own recounting of the procedure, the patient stayed with the McDowell family for 25 days after which she then again horseback rode 60 miles back to her home, in the middle of winter. Apparently these two protagonists never met again and Mrs. Crawford survived Dr. McDowell for at least 13 years. More information on the patient can be found in this article.
Dr. McDowell was a very religious man and the night before the operation he wrote a prayer that he kept in his pocket during the operation. Following is the text of the prayer. If you visit a store across the street from the McDowell House and Museum you can buy a facsimile of the prayer.
The Prayer
"Almighty God be with me I humbly beseech Thee, in this attendance in Thy holy hour; give me becoming awe of Thy presence, grant me Thy direction and aid, I beseech Thee, that in confessing I may be humble and truly penitent in prayer, serious and devout in praises, grateful and sincere, and in hearing Thy word attentive, and willing and desirous to be instructed. Direct me, oh! God, in performing this operation, for I am but an instrument in Thy hands, and am but Thy servant, and if it is Thy will, oh! spare this poor afflicted woman. Oh! give me true faith in the atonement of Thy Son, Jesus Christ, or a love sufficient to procure Thy favor and blessing; that worshipping Thee in spirit and in truth my services may be accepted through his all-sufficient merit. Amen."
Dr. McDowell only published the operation and its results in 1817. In several biographies that I have read it is stated that many were envious and jealous of his accomplishments to the point of creating tales that he “cut women open to murder them”. In her granddaughter’s biography or her illustrious grandfather she writes: “McDowell was conscious at the time he was doing the operation, that an angry and excited crowd of men were collected in the street awaiting the result of his experiment of "butchering a woman," as they expressed it. Had she died under the operation, there was no law in those primitive days sufficiently strong to have protected him from the people who were clamoring for his life—determined men who would have shown no mercy, for they regarded it a duty to avenge the wrong inflicted on Mrs. Crawford. Indeed his life hung on the recovery of the heroic woman.”
NOTE: Not long after I wrote this article, I came across a biography book of Dr. McDowell; inside it I found a copy of this prayer owned by Dr. Robert Thompson, along with a copy of a letter From Dr. McDowell addressed to Dr. Thompson with a description of the procedure.
Sources:
1. “Ephraim McDowell and Jane Todd Crawford, the Bicentennial of a Surgical Masterpiece” Benigno, BB Obst & Gynecol (2009) 113. 5:1141-1144
2. “The Biography of Ephraim McDowell, M.D.; The Father of Ovariotomy” Ridenbaugh, MY, 1890 CL Webster & Co.
3. “Ephraim McDowell: "Father of ovariotomy" and founder of abdominal surgery, with an appendix on Jane Todd Crawford” Schachner, A 1921, J.B. Lippincott Co.
- Details
The following is an article published by Theo Dirix in his blog. He is one of the Vesalius Continuum project members and a contributor to this website. Theo Dirixis an author and a taphophile. He has successively held the office of Consul in Embassies of Belgium in Tanzania, Saudi Arabia, Jordan, Canada, the United Arab Emirates and, since 2011, Greece. His current posting is in Kopenhagen, Denmark Before 1989, he worked for the Flemish Radio 3 and commented on (mainly Moroccan) literature. He is constantly writing travel stories of his visits to cemeteries and graves. He is also the author of the book "In Search of Andreas Vesalius: The Quest for the Lost Grave".
Isn’t it amazing how much we know about a scientist and physician who lived five hundred years ago, I am referring, of course, to the prominent figure of Andreas Vesalius (1514-1564)? (2)
After a jump start in academia in Italy, the Flemish anatomist made a sudden career move and became the family physician of Charles V, Emperor of the Holy Roman Empire, and to his successor Philip II and their powerful entourage in Spain. His brilliant early work, De Humani Corporis Fabrica Libri Septem, a milestone in the transition to empiric research, which has a revolutionary pedagogical and artistic approach, still inspires.
Isn’t it even more amazing that new discoveries about this giant and his achievements steadily continue to surface?(3) Most amazing, though, is that several hoaxes, mainly about his final months and days, doggedly survive.(4) Where is that undeniable proof that he ever ran into the otherwise so well documented inquisition?(5) Vesalius left Spain as a pious pilgrim. A laissez-passer [safe passage document] by Philip II and letters from the Spanish Embassy in Venice are conserved in archives in Spain. Even the thanking note by the Custodian of the Holy Places in Jerusalem, which Vesalius was to hand over to Philip II, reached its destination.(6) That unequivocally refutes the other obstinate prank that a shipwreck during his return was the cause of his death.
Some now argue that scurvy may have been the cause; Omer Steeno, Maurits Biesbrouck and Theodoor Goddeeris point in the direction of general fatigue.(7) Obviously, only the discovery of his remains will help determine why he collapsed on the quay of Zakynthos (Greece), then a Venetian colony, as described in a recently rediscovered eyewitness report.(8) He was buried in the local catholic church of Santa Maria delle Grazie. Several Jerusalem pilgrims have indeed described his epitaph. Unfortunately, the church has disappeared. During its history, it was sacked, abandoned, damaged and finally, after major earthquake in 1953, bulldozed into the sea.
In view of the quincentenary of the anatomist, medical artist Pascale Pollier, hoping to reconstruct his face from his cranium, started a romantic quest for his remains. Under the impetus of the author and the Embassy of Belgium in Athens, archaeologists have been involved: Prof. Jan Driessen, Université Catholique de Louvain (UCL) and Director of the Belgian School in Athens, EBSA, and Apostolos Sarris, Deputy Director of the Institute for Mediterranean Studies - Foundation for Research and Technology, Hellas (IMS-FORTH).
In 2014, Dr. Sylviane Déderix (UCL/IMS-FORTH) checked the presumed location of the church through the spatial analysis of a Geographical Information System (GIS). With that digital tool, she displayed, corrected and analysed historical maps on modern cartographic data. The result confirms that the ruins of the Santa Maria delle Grazie and its annexes are to be found to the northwest of the intersection of Kolyva Street and Kolokotroni Street, partly below the asphalt and partly under private property of emergency lodgings, which date from the ’53 earthquake, and partly under a fairly new construction.
To enrich the GIS of the first phase, a geophysical approach of anomalies under the surface should now follow. In this urban environment only non-destructive methods like ground penetrating radar (GPR) and electrical resistivity tomography (ERT) can be carried out. With the necessary permissions and funding, a team of researchers could be deployed to collect and process such data. If these are conclusive, a third phase of small scale excavations in search of remains may follow. To top up personal investments, Vesalius Continuum(9) has launched a crowd funding campaign to sponsor the second phase. If you wish to contribute to finding the real cause of Vesalius’s death and help Pascalle Pollier reconstruct the face of a genius whose legacy survives to this very day, visit: www.gofundme.com/VesaliusContinuum
Personal note: Click on the following link to collaborate with this incredible quest. I already did. Dr. Miranda
Notes and Sources:
(1) The author thanks Maurits Biesbrouck, Sylviane Déderix, Jan Driessen, Theodoor Goddeeris, Akis Ladikos, Pavlos Plessas, Pascale Pollier, Apostolos Sarris, Maria Sidirokastriti - Kontoni and Omer Steeno.
(2) Maurits Biesbrouck upgraded Dr. Harvey Cushing’s list of publications on Vesalius to more than 3000 records: http://www.andreasvesalius.be , accessed 8 January 2017.
(3) In 2007 a Canadian book collector bought Vesalius’ own copy of the 1555 edition of the Fabrica, heavily annotated in preparation of a never published third edition. In 2014 Vesalius’ own annotated copy of Institutiones by his teacher, J.G. von Andernach, came to light.
(4) DIRIX, Theo: Andreas Vesalius and his hoaxes, con variazioni, in: Vesalius, Journal of the International Society of the History of Medicine, Vol. XXII, nr. 1, June 2016, Special Issue, Proceedings of A Tribute to Andreas Vesalius, Padua, Italy - December 2015, pp. 103 - 111.
(5) The source is post-mortem gossip spread in January 1565 by the French diplomat, Hubertus Languetus, in a note of 24 lines opening with: “rumour has it”. See: BIESBROUCK, Maurits, Theodoor GODDEERIS, Omer STEENO. ‘Post Mortem’ Andreae Vesalii (1514-1564), Deel I. De laatste reis van Andreas Vesalius en de omstandigheden van zijn dood), in: A.Vesalius, nr. 3 september 2015, Alfagen, Leuven, pp 154-161.
(6) In total four letters have been discovered by José Baron Fernandez in the archives of Simancas, described and published since 1965
(7) BIESBROUCK, Maurits, Theodoor GODDEERIS, Omer STEENO. ‘Post Mortem’ Andreae Vesalii (1514-1564), Deel II. Het graf van Andreas Vesalius op Zakynthos, (vervolg en slot na Deel I in vorig nummer), in: A.Vesalius, nr. 4 december 2015, Alfagen, Leuven, pp 193-200.
(8) ibid
(9) Within the initial ad hoc organising committee of the Vesalius Continuum Conference in September 2014 in Zakynthos, medical artist Pascale Pollier and the author, then Consul at the Embassy of Belgium in Athens, formed the Search team. See: DIRIX, Theo, In Search of Andreas Vesalius, The Quest for the Lost Grave, LannooCampus, Leuven, 2014.
GoFundMe Campaign for the next stage of the project
- Details
This article is part of the series "A Moment in History" where we honor those who have contributed to the growth of medical knowledge in the areas of anatomy, medicine, surgery, and medical research.
This is the continuation of the article “The Ephraim McDowell House and Museum (1)”
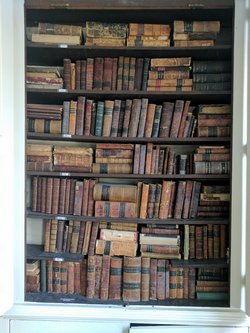
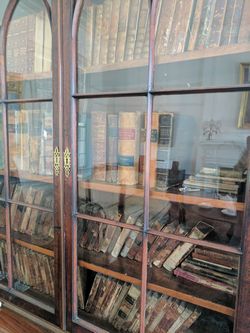
The first room we visited from the foyer was the library. Antique furniture, elegant oil lamps and in wooden built-in-the-wall shelfs an incredible collection of antique books from the 1700-1900’s covering everything from medicine and surgery to history, philosophy and poetry. One of the shelves pictured here had mostly medical books.
As a book collector I was so tempted to touch, open, and read some of the books, but they are only for display. I could recognize some of the books as items that I would like to own and place in my library. The docent explained that, as the custom of the times, the library was the place for men to meet, smoke, read, share a bourbon, and discuss the events and politics of the day.
The next room was the music room. Dr. McDowell played the violin while his wife played the piano, both on display as well as other antique instruments donated to the museum. Antique furniture and over the fireplace mantle two whale oil lamps. There are family portraits all over the house. One can almost imagine the life of the times…
Interestingly, there is a large wooden door that opens from the foyer to the patio. The guide explained that it was a “casket door” so that people who died in the house could be taken through the door to the back of the house and not through the front door.
A wooden staircase leads to the second floor, where there is a small bedroom that was for the children. Because of the number of children, they had to sleep two or three to a bed. There is furniture, antique bedspreads, bedpans (there were no bathrooms in the house), even some toys, dolls, and chalk tablets.
The master bedroom is also on the second floor. Larger and more spacious, it was the place where women would get together to talk, knit and quilt. On the mantelpiece there is a family sword.
The next room is the “operating room” where history was made on Christmas Day, 1809.
- Details
This article is part of the series "A Moment in History" where we honor those who have contributed to the growth of medical knowledge in the areas of anatomy, medicine, surgery, and medical research.
In 2013 I wrote a short biography of Dr. Ephraim McDowell (1771- 1830) for the sidebar on this blog entitled “A Moment in History”. While researching the life of this illustrious surgeon I learned that his house is now a National Historic Landmark and has been transformed into a museum in the city of Danville, Kentucky. It took me almost four years but on Sunday February 19, 2017 I was able to go visit this place. Following is a series of articles and pictures of this visit.
The house itself was built in the 1790’s and most of it has been restored and lovingly maintained by the city, the Kentucky Medical Association, a Board of Directors, and a group of volunteers that work as docents giving tours of the house.
The following is an edited excerpt of Wikipedia on the McDowell House:
“After McDowell's death in 1830 the house was sold. It was the home of a Centre College president for a short time. Later the entire area became a slum and tenement property. The house deteriorated badly. Dr. August Schachner, of Louisville, led the efforts to buy the house for restoration. In 1921 he visited the house. "Since our last visit, the house has continued its downward course until it has reached a point where it now seems almost beyond redemption”. The room in the rear of the corresponding front room on the second floor,"(the operating room) "which is on a lower level by several feet, is used as a dump for the ashes from the grates of the rooms on the second floor."
The Kentucky Medical Association bought the house in 1935 and deeded it to the state of Kentucky, who had it restored by the Works Progress Administration (WPA). It was dedicated on May 20, 1939. In 1948, Kentucky returned the property to the Kentucky Medical Association.
The Kentucky Pharmaceutical Society restored the Apothecary Shop in the late 1950s with help from the Eli Lily Foundation. It was furnished by the Pfizer Laboratories. It was dedicated and presented to the Kentucky Medical Association on August 14, 1959.”
The house is located at 125 South Second Street, Danville, KY 40422. It is a white two-story wooden structure considered to be large for the time. To the right side stands a small one-story brick structure, the apothecary, where Dr. McDowell would provide medicine for his patients and others. To the left is the patio and garden where Dr. McDowell would grow medicinal plants for the apothecary. On the garden front there is a large two-sided plaque that reads:
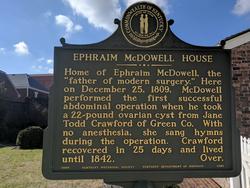
Front of the plaque at the Ephraim McDowell House
“Home of Ephraim McDowell, the “father of modern surgery.” Here on December 25, 1809 McDowell performed the first successful abdominal operation when he took a 22-pound ovarian cysts from Jane Todd Crawford of Green Co. With no anesthesia, she sang hymns during the operation. Crawford recovered in 25 days and lived until 1842”

Back of the plaque at the Ephraim McDowell House
“Built in three stages. Brick ell, or single-story wing, built 1790s. McDowell purchased house in 1802 and added front clapboard section c.1804. Rear brick office and formal gardens added in 1820. House sold when McDowell dies in 1830. 1n 1930s, Ky. Med. Assoc. bought house; restored by WPA. House dedicated on May 20, 1939. Now a house museum”
- Details
This is a series of articles on depression published as a community service. The information in these articles follow our Privacy and Security Guidelines and cannot be construed as medical guidance. For additional information and counseling, consult with your physician or the appropriate health care professional of your choice. You can also find information on Transcranial Magnetic Stimulation (TMS) here. For the initial article on this series click here.
This article could also be entitled:
What is the difference between unipolar and bipolar depression?
Mood is a range of emotions that describe how we "feel" at a particular point in time. Mood is called a "visceral" (gut-like) sensation and is difficult to describe. It is a sensation dependent on a group of deep brain structures known as the limbic system.
Being a spectrum, there are two ends or "poles" to the range. An one end we have the major depressive mood of darkness, despair, and loathing of one's self. At the other end or "pole" we have the manic feeling of happiness, feeling "high", with extreme irritability and quick actions without measuring potential consequences.
An MDD patient that is "stuck" at the dark end of the spectrum, is said to be "unipolar", as the Latin word unus and uni- mean "one". The patient is always at one pole, therefore "unipolar".
Some depression patients have mood swings going from one end of the mood spectrum to the other. Since the medical prefix [bi-] means "two", these patients are said to have a "bipolar" type depression.
Some authors comment that there is not really a true unipolar depression for even unipolar depression patients move within the mood spectrum as their pathology evolves with treatment.
Experience tells us that as a depression patient starts to come out of their neurologically depressed state they may begin to show anxiety. This is easily treated by adding a secondary prescription course of right-sided low frequency treatment of TMS. As you go through your TMS Therapy treatment you may expect your prescription and dosage to change to accommodate your development towards a life without depression
References:
1. Barbee, J. G. (1998). Mixed symptoms and syndromes of anxiety and depression: Diagnostic, prognostic, and etiologic issues. Annals of Clinical Psychiatry, 10:15–29.
2. Regier, D. A., Rae, D. S., Narrow, W. E., Kaelber, C. T., & Schatzberg, A. F. (1998). Prevalence of anxiety disorders and their comorbidity with mood and addictive disorders. British Journal of Psychiatry. Supplement, 34: 24–28.