Medical Terminology Daily (MTD) is a blog sponsored by Clinical Anatomy Associates, Inc. as a service to the medical community. We post anatomical, medical or surgical terms, their meaning and usage, as well as biographical notes on anatomists, surgeons, and researchers through the ages. Be warned that some of the images used depict human anatomical specimens.
You are welcome to submit questions and suggestions using our "Contact Us" form. The information on this blog follows the terms on our "Privacy and Security Statement" and cannot be construed as medical guidance or instructions for treatment.
We have 1132 guests and no members online

Jean George Bachmann
(1877 – 1959)
French physician–physiologist whose experimental work in the early twentieth century provided the first clear functional description of a preferential interatrial conduction pathway. This structure, eponymically named “Bachmann’s bundle”, plays a central role in normal atrial activation and in the pathophysiology of interatrial block and atrial arrhythmias.
As a young man, Bachmann served as a merchant sailor, crossing the Atlantic multiple times. He emigrated to the United States in 1902 and earned his medical degree at the top of his class from Jefferson Medical College in Philadelphia in 1907. He stayed at this Medical College as a demonstrator and physiologist. In 1910, he joined Emory University in Atlanta. Between 1917 -1918 he served as a medical officer in the US Army. He retired from Emory in 1947 and continued his private medical practice until his death in 1959.
On the personal side, Bachmann was a man of many talents: a polyglot, he was fluent in German, French, Spanish and English. He was a chef in his own right and occasionally worked as a chef in international hotels. In fact, he paid his tuition at Jefferson Medical College, working both as a chef and as a language tutor.
The intrinsic cardiac conduction system was a major focus of cardiovascular research in the late nineteenth and early twentieth centuries. The atrioventricular (AV) node was discovered and described by Sunao Tawara and Karl Albert Aschoff in 1906, and the sinoatrial node by Arthur Keith and Martin Flack in 1907.
While the connections that distribute the electrical impulse from the AV node to the ventricles were known through the works of Wilhelm His Jr, in 1893 and Jan Evangelista Purkinje in 1839, the mechanism by which electrical impulses spread between the atria remained uncertain.
In 1916 Bachmann published a paper titled “The Inter-Auricular Time Interval” in the American Journal of Physiology. Bachmann measured activation times between the right and left atria and demonstrated that interruption of a distinct anterior interatrial muscular band resulted in delayed left atrial activation. He concluded that this band constituted the principal route for rapid interatrial conduction.
Subsequent anatomical and electrophysiological studies confirmed the importance of the structure described by Bachmann, which came to bear his name. Bachmann’s bundle is now recognized as a key determinant of atrial activation patterns, and its dysfunction is associated with interatrial block, atrial fibrillation, and abnormal P-wave morphology. His work remains foundational in both basic cardiac anatomy and clinical electrophysiology.
Sources and references
1. Bachmann G. “The inter-auricular time interval”. Am J Physiol. 1916;41:309–320.
2. Hurst JW. “Profiles in Cardiology: Jean George Bachmann (1877–1959)”. Clin Cardiol. 1987;10:185–187.
3. Lemery R, Guiraudon G, Veinot JP. “Anatomic description of Bachmann’s bundle and its relation to the atrial septum”. Am J Cardiol. 2003;91:148–152.
4. "Remembering the canonical discoverers of the core components of the mammalian cardiac conduction system: Keith and Flack, Aschoff and Tawara, His, and Purkinje" Icilio Cavero and Henry Holzgrefe Advances in Physiology Education 2022 46:4, 549-579.
5. Knol WG, de Vos CB, Crijns HJGM, et al. “The Bachmann bundle and interatrial conduction” Heart Rhythm. 2019;16:127–133.
6. “Iatrogenic biatrial flutter. The role of the Bachmann’s bundle” Constán E.; García F., Linde, A.. Complejo Hospitalario de Jaén, Jaén. Spain
7. Keith A, Flack M. The form and nature of the muscular connections between the primary divisions of the vertebrate heart. J Anat Physiol 41: 172–189, 1907.
"Clinical Anatomy Associates, Inc., and the contributors of "Medical Terminology Daily" wish to thank all individuals who donate their bodies and tissues for the advancement of education and research”.
Click here for more information
- Details

Image courtesy of Ancient Touch
UPDATED: The word [glenoid] is composed of the root term [-glen-] which arises from the Greek [γλήνη] (glíni), meaning “a shallow socket”, and the suffix [-oid], also Greek, meaning “similar to”. Similar to a shallow socket.
The etymology of the word is not clear, as some authors contend that it means “eyeball” or just the “pupil” of the eye. The earliest known use of the term by Homer was referring to a “mirror”. All of these meanings carry the reference to reflection of an image.
The term [glenoid cavity] is the smooth, slightly concave surface of the glenoid process of the scapula that forms part of the shoulder joint. Being so shallow, the glenoid cavity is supplemented by a fibrocartilaginous ring called the [glenoid labrum]. There are other uses of the term [glenoid] in human anatomy.
Personal note: I have read several authors including Skinner (1970) on this word. I noticed that ancient Greek mirrors have one very slightly concave surface (see image) and this could be the origin of this term as well as the later association with reflection. Dr. Miranda
Original image courtesy of www.ancienttouch.com
- Details
- Written by: Fernanda Cortes, DDS, MSc
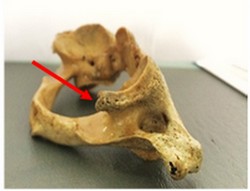
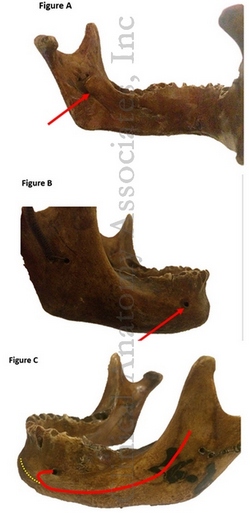
Figure A: Incomplete PP viewed from the
posterior aspect of the articular fossa
related to the retroglenoid tubercle
The Ponticulus Posticus (PP), also known as the pons arcuatus, foramen arcuale, and arcuate foramen, is a bony bridge that connects the retroglenoid tubercle with the posterior arch of the C1 vertebra, also known as the Atlas.
It substitutes the lateral segment of the posterior atlantooccipital ligament or joint capsule (1) on the area which stabilizes the vertebral artery on its emergency of the transverse foramen of the Atlas (2). This bridge or arch could be thick, thin or even incomplete (2). The importance of this calcification relies on the fact that it has been linked with cervicogenic headache (1,3) chronic tension-type headaches, sensorineural hearing loss (4), shoulder and arm pain, neck pain, and vertigo (1, 5).
The presence of a ponticulus posticus could also impact the planning of high cervical surgeries associated with the Atlas [C1] (6). A recent meta-analysis of the prevalence of this condition worldwide found an overall prevalence of a complete PP of 9.1% versus an incomplete PP, which was 13.6%. In males (10.4%) the complete PP was more common than in females (7.3%), but an incomplete PP was more commonly seen in females (18.5%) than in males (16.7%) (7).

Figure B: Complete PP. It crosses from the
retroglenoid tubercle down to the
posterior arch.
Despite the fact that this calcification has been associated with different painful disorders, some other authors consider it an anatomical condition destined to protect the vertebral artery and not a pathological condition (8). PP is visible on lateral cervical spine and cranial lateral radiographs as thin bony arch on the shape of a ring crossing from the retroglenoid tubercle to the posterior arch of C1, being either partially of fully calcified (Figures C and D).
Note 1: For the etymology of the term glenoid, click here.
Note 2: Figures C and D can be found at the bottom of the article
Sources:
1. Ross JS, Moore KR, editors. Diagnostic Imaging: Spine E-Book. 3rd ed. Philadeplphia: Elsevier; 2015. 31 p.
2. Torres Cueco R. La Columna Cervical: Evaluación Clínica y Aproximaciones Terapéuticas. Principios anatómicos, funcionales, exploración clínica y técnicas de tratamiento. Tomo I. 1° Ed. Madrid: Medica Panamericana; 2008. 124 p.
3. Tambawala SS, Karjodkar FR, Sansare K, Motghare D, Mishra I, Gaikwad S, Dora AC. Prevalence of Ponticulus Posticus on Lateral Cephalometric Radiographs, its Association with Cervicogenic Headache and a Review of Literature. World Neurosurg [Internet]. 2017 Apr 17(cited 02 Jun 2017). pii: S1878-8750(17)30525-9. Available at: doi: 10.1016/j.wneu.2017.04.030. [Epub ahead of print]
4. Koutsouraki E, Avdelidi E, Michmizos D, Kapsali SE, Costa V, Baloyannis S. Kimmerle's anomaly as a possible causative factor of chronic tension-type headaches and neurosensory hearing loss: Case report and literature review. Int J Neurosci. 2010; 120:236-9
5. Cakmak O, Gurdal E, Ekinci G, Yildiz E, Cavdar S. Arcuate foramen and its clinical significance. Saudi Med J. 2005; 26:1409-13.
6. Song MS, Lee HJ, Kim JT, Kim JH, Hong JT. Ponticulus posticus: Morphometric analysis and Its anatomical Implications for occipito-cervical fusion. Clin Neurol Neurosurg [Internet]. 2017 Jun (cited 02 Jun 2017);157:76-81. Available at: doi: 10.1016/j.clineuro.2017.04.001. Epub 2017 Apr 3.
7. Pękala PA, Henry BM, Pękala JR, Hsieh WC, Vikse J, Sanna B, Walocha JA, Tubbs RS, Tomaszewski KA. Prevalence of foramen arcuale and its clinical significance: a meta-analysis of 55,985 subjects. J Neurosurg Spine [Internet]. 2017 Jun (cited 02 Jun 2017); 16:1-15. Available at: doi: 10.3171/2017.1.SPINE161092. [Epub ahead of print]
8. Schilling J, Schilling A, Suazo I. Ponticulus posticus on the Posterior Arch of Atlas, Prevalence Analysis in Asymptomatic PatientsInt. J. Morphol. 2010 Mar; 28(1):317-322.
Acknowledgments: The Atlas [C1] specimens shown on figures A and B belong to the Anatomy department of the Medical College of the Finis Terrae University, Santiago, Chile and are used to show two examples of PP. With permission.
Article written by Prof. M. Fernanda Cortes, DDS, MsC.
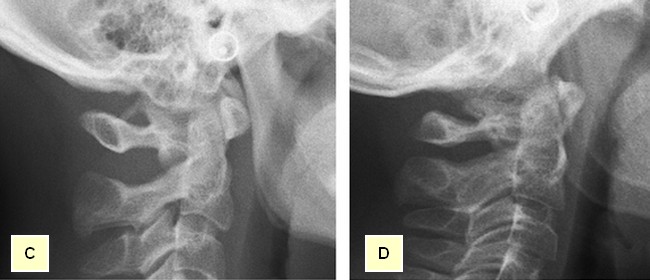 Figure C: Complete PP shown on a lateral radiographic view. Figure D: Partial PP shown on a lateral radiographic view.
Figure C: Complete PP shown on a lateral radiographic view. Figure D: Partial PP shown on a lateral radiographic view.
- Details

Wax bust of Andreas Vesalius by Pascale Pollier
Friends of Medical Terminology Daily:
As you know, we are part of an incredible quest to find the body of Andreas Vesalius, recognized worldwide as the Father of Modern Anatomy. His life and the story and legends about his death are part now of scientific fact and folklore.
The quest for the lost grave of Andreas Vesalius has been published in this blog several times. Many of the members of this group, such as Pascale Pollier, Theo Dirix, Dr. Sylvianne Déderix, Dr. Maurits Biesbrouck, etc. are contributors to Medical Terminology Daily.
The project has had several stages and you are welcome to follow the above links to the authors to read their contributions which clarify the scope and objectives of this quest, including Theo Dirix's article : "To put it in another way: where do we have to look for Vesalius's grave?".
The project next step is to perform a detailed research on the area where we suspect (actually know with a high degree of certainty) where the cemetery of the Church of Santa Maria delle Grazie (Zakynthos, Greece) used to be.

Church of Santa Maria delle Grazie
The problem was to obtain the permits to do the non-invasive radar scan of the grounds in the area... and this is the exciting news! Following is the press release:
"The Belgian School of Archaeology)in Athens (EBSA) just obtained the permission for a new archaeological project at Zakynthos in collaboration with the local Ephorate and Dr Merkouri, as well as the IMS in Rethymnon (Dr A. Sarris). The project, initiated and coordinated by Theo Dirix and Pascale Pollier, concerns the quest for the tomb of the Belgian anatomist, father of modern anatomy, Andreas Vesalius who died and was buried in the island."
Needless to say, we are all excited. Now we have to fund this research, and you can all help by contributing as little or as much as you can to the GoFundMe page. We are very close to our objective and this will allow us to pay the permits, rent the equipment and finally get a little closer to finding Andreas Vesalius.
Personal note: Click on the following link to collaborate with this incredible quest. I already did. Dr. Miranda
GoFundMe Campaign for the next stage of the project
- Details
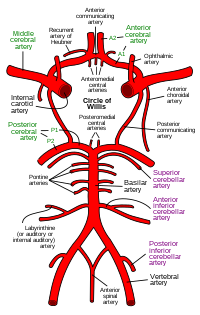
UPDATED: The arterial "circle of Willis" is a roundabout of arteries found at the base of the brain, allowing for collateral circulation at this level. This arterial circle has been described by many anatomists, but it was Thomas Willis (1621 - 1675) who described it in most detail, and he was the first to understand its function.
The circle of Willis receives blood from the two main paired arteries that provide blood supply to the head and brain: the carotid arteries anteriorly, and the vertebral arteries posteriorly.
This arterial circle is formed by the anastomosis of several arteries, paired and unpaired:
• Anterior cerebral arteries: These paired arteries are one of the terminal branches of the internal carotid arteries. They provide blood supply to the medial aspect and part of the lateral aspect of frontal and parietal lobes of the brain
• Anterior communicating artery: A single unpaired small artery communicating both anterior cerebral arteries and providing potential collateral circulation between them
• Internal carotid arteries: These two bilateral arteries are one of the branches of the carotid artery found at the root of the neck. Its two main terminal branches are the anterior cerebral arteries and the middle cerebral arteries.
• Posterior cerebral arteries: These two arteries are formed by the bifurcation of the basilar artery, which itself is formed by the junction of the right and left vertebral arteries. The posterior cerebral arteries provide blood supply to the occipital lobe and part of the temporal lobe of the brain
• Posterior communicating arteries: These paired arteries provide communication between the carotid and vertebral arterial territories
• Middle cerebral arteries: Although not technically part of the arterial circle of Willis, these paired arteries are one of the two terminal branches of the internal carotid arteries. The middle cerebral artery travels deep in the lateral sulcus (Sylvian fissure) of the brain and provides blood supply to the lateral aspect of the brain including the frontal, parietal, occipital, temporal, and insular lobes
The arterial circle of Willis provides all of the arterial blood to the brain. Cerebral blood flow in humans averages 55 mL per 100 g of brain tissue per minute. This is a about over 742.5 mL/min for the average 1350 g brain. Depending on the situation the brain will use between 15 to 20 percent of the total cardiac output, although by weight the brain is only about two to three percent of the average body weight. Incredibly, the brain uses more oxygen that most organs averaging close to 25% of the total oxygen needs of the body!
The importance of the arterial circle of Willis is that beyond this point the arterial supply to the brain becomes terminal, that is, there are little or no anastomoses between the bifurcating branches exposing the brain to ischemia and necrosis should there be an arterial stenosis or stricture. The circle of Willis is an area prone to aneurysms, with over 27,000 cases yearly in the US.
For an image of the vascular territories of the brain, click here.
Thanks to Jackie Miranda-Klein for making me review this post and update it!... and congratulations to Jackie for starting her Physician Assistant Master's degree at Kettering College. Dr. Miranda.
Image in the Public Domain. Courtesy of www.wikipedia.org
Clinical anatomy, pathology, and surgery of the brain and spinal cord are some of the lecture topics developed and delivered by Clinical Anatomy Associates, Inc.
- Details
- Written by: Fernanda Cortes, DDS, MSc
The mandibular canal is a long, bilateral canal which runs along and within the mandible. This canal transports the inferior alveolar neurovascular bundle. The mandible is known vernacularly as the “jawbone” or “lower jaw”.
The mandibular canal starts on the medial surface of the mandibular ramus at the mandibular foramen (Figure A, arrow) descends anteroinferiorly through the body of the mandible until it ends in the mental foramen at the buccal (anterior) surface of the mandible, usually in the area between the premolars (Figure B, arrow).
Before exiting, the canal forms an “anterior loop” projected anterior to the mental foramen prior to changing its direction back and outwards in direction to the buccal plate (Figure C, red line). This last portion of the canal is called the “mental canal”.
A frequent anatomical variation is the presence of a bifid mandibular canal (recent studies indicate it has a prevalence of around 16%).
Different anatomical studies show that the mandibular canal not only finishes at the mental foramen, but it could divide itself giving an incisive canal which runs anteriorly onto the incisal region (Figure C, yellow line). When it doesn’t continue as an incisal canal, the neurovascular elements go anteriorly through the cells of the spongy bone tissue.
The presence of this Incisal canal has surgical relevance, and knowledge of its exact location and anatomical parameters has a high importance on reducing complications of surgical procedures in the mental area such as dental implants, bone lesions removal and bone harvesting among others, all which could damage the incisal canal and the neurovascular bundle inside it.
With the latest use of CBCT (Cone Beam Computed Tomography) technology to evaluate anatomical structures, the presence of this canal has showed to be high (92-100%) and its length can vary from reaching only the premolar area or even the central mandibular incisors in the least of cases.
Sources:
1. Haas LF, Dutra K, Porporatti AL, Mezzomo LA, De Luca Canto G, Flores-Mir C, Corrêa M. Anatomical variations of mandibular canal detected by panoramic radiography and CT: a systematic review and meta-analysis. Dentomaxillofac Radiol. 2016;45(2):20150310.
2. Kong N, Hui M, Miao F, Yuan H, Du Y, Chen N. Mandibular incisive canal in Han Chinese using cone beam computed tomography. Surg Radiol Anat. 2016 Nov 11. [Epub ahead of print] Int J Oral Maxillofac Surg. 2016 Sep;45(9):1142-6.
3. Rouvierre H, Delmas A. Anatomía humana: Descriptiva, topográfica y funcional. Cabeza y cuello. Volumen 1. 11° ed. España: Masson, S.A.;2005. P. 114.
4. Von Arx T, Lozanoff S. Clinical Oral Anatomy: A Comprehensive Review for Dental Practitioners and researchers. Switzerland: Springer; 2016. P 323- 390
Article and image provided by Prof. M. Fernanda Cortes, DDS, MsC.
- Details
- Written by: Efrain A. Miranda, Ph.D.
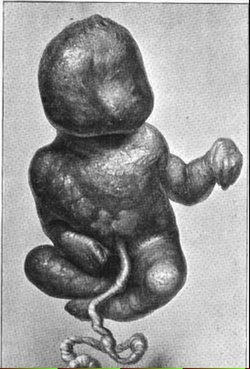
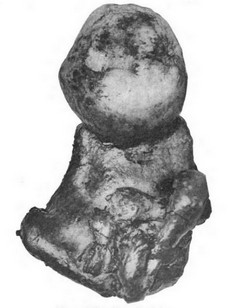
This word originates from the root terms [-lith-], which arises from the Greek word [λίθος] meaning “stone” and the term [-pedion-] (or [pædion]) which is also Greek [παιδί] meaning “child”. In simple terms this would mean a “stone child”.
Strangely enough, “stone children” or lithopædia are rare cases found in nature, and have been described in humans since early times, the first one by Abū al-Qāsim (Abulcasis) in the 10th century.
When found, it is usually a fetus of more than 12 weeks of estimated age. This is because a younger fetus, if it dies, will usually be reabsorbed by the mother’s body. Usually they are ectopic pregnancies where the fetus dies and is calcified, turning into “stone”.
Technically there are three types of lithopaedia:
1. Lithokelyphos: Only the surrounding fetal membranes calcify. The fetus decomposes and is absorbed, while the calcified membranes protect the mother from the effects of necrosis.
2. Lithokelyphopaedion: Where the membranes and the fetus calcify.
3. True lithopedion, also known as “lithopedion proper”, or lithotecnon. The most common presentation when found, only the fetus is calcified.
The incidence of lithopedia is estimated close to 1.8% of ectopic pregnancies. The following images are of a lithopedion case described by Bainbridge in 1911 and include an X-Ray of the lithopedion.
Sources:
1. “A rare case of Lithopedion” Clark, JG John Hopkins Hospital Bulletin Volume 8 (1897) 221-228
2. “Lithopedion, Report of a case with a review of the literature” Bainbridge, WS. Am J Obstr V65 (1911) 31 – 52
3. “Chilean woman carried calcified foetus for 50 years” BBC News
4. Blog: James Edwards Hughes “The Lithopedion”