Medical Terminology Daily (MTD) is a blog sponsored by Clinical Anatomy Associates, Inc. as a service to the medical community. We post anatomical, medical or surgical terms, their meaning and usage, as well as biographical notes on anatomists, surgeons, and researchers through the ages. Be warned that some of the images used depict human anatomical specimens.
You are welcome to submit questions and suggestions using our "Contact Us" form. The information on this blog follows the terms on our "Privacy and Security Statement" and cannot be construed as medical guidance or instructions for treatment.
We have 725 guests online

Jean George Bachmann
(1877 – 1959)
French physician–physiologist whose experimental work in the early twentieth century provided the first clear functional description of a preferential interatrial conduction pathway. This structure, eponymically named “Bachmann’s bundle”, plays a central role in normal atrial activation and in the pathophysiology of interatrial block and atrial arrhythmias.
As a young man, Bachmann served as a merchant sailor, crossing the Atlantic multiple times. He emigrated to the United States in 1902 and earned his medical degree at the top of his class from Jefferson Medical College in Philadelphia in 1907. He stayed at this Medical College as a demonstrator and physiologist. In 1910, he joined Emory University in Atlanta. Between 1917 -1918 he served as a medical officer in the US Army. He retired from Emory in 1947 and continued his private medical practice until his death in 1959.
On the personal side, Bachmann was a man of many talents: a polyglot, he was fluent in German, French, Spanish and English. He was a chef in his own right and occasionally worked as a chef in international hotels. In fact, he paid his tuition at Jefferson Medical College, working both as a chef and as a language tutor.
The intrinsic cardiac conduction system was a major focus of cardiovascular research in the late nineteenth and early twentieth centuries. The atrioventricular (AV) node was discovered and described by Sunao Tawara and Karl Albert Aschoff in 1906, and the sinoatrial node by Arthur Keith and Martin Flack in 1907.
While the connections that distribute the electrical impulse from the AV node to the ventricles were known through the works of Wilhelm His Jr, in 1893 and Jan Evangelista Purkinje in 1839, the mechanism by which electrical impulses spread between the atria remained uncertain.
In 1916 Bachmann published a paper titled “The Inter-Auricular Time Interval” in the American Journal of Physiology. Bachmann measured activation times between the right and left atria and demonstrated that interruption of a distinct anterior interatrial muscular band resulted in delayed left atrial activation. He concluded that this band constituted the principal route for rapid interatrial conduction.
Subsequent anatomical and electrophysiological studies confirmed the importance of the structure described by Bachmann, which came to bear his name. Bachmann’s bundle is now recognized as a key determinant of atrial activation patterns, and its dysfunction is associated with interatrial block, atrial fibrillation, and abnormal P-wave morphology. His work remains foundational in both basic cardiac anatomy and clinical electrophysiology.
Sources and references
1. Bachmann G. “The inter-auricular time interval”. Am J Physiol. 1916;41:309–320.
2. Hurst JW. “Profiles in Cardiology: Jean George Bachmann (1877–1959)”. Clin Cardiol. 1987;10:185–187.
3. Lemery R, Guiraudon G, Veinot JP. “Anatomic description of Bachmann’s bundle and its relation to the atrial septum”. Am J Cardiol. 2003;91:148–152.
4. "Remembering the canonical discoverers of the core components of the mammalian cardiac conduction system: Keith and Flack, Aschoff and Tawara, His, and Purkinje" Icilio Cavero and Henry Holzgrefe Advances in Physiology Education 2022 46:4, 549-579.
5. Knol WG, de Vos CB, Crijns HJGM, et al. “The Bachmann bundle and interatrial conduction” Heart Rhythm. 2019;16:127–133.
6. “Iatrogenic biatrial flutter. The role of the Bachmann’s bundle” Constán E.; García F., Linde, A.. Complejo Hospitalario de Jaén, Jaén. Spain
7. Keith A, Flack M. The form and nature of the muscular connections between the primary divisions of the vertebrate heart. J Anat Physiol 41: 172–189, 1907.
"Clinical Anatomy Associates, Inc., and the contributors of "Medical Terminology Daily" wish to thank all individuals who donate their bodies and tissues for the advancement of education and research”.
Click here for more information
- Details
The Billroth I procedure was pioneered by Dr. Theodor Billroth in 1881. The original procedure was described as a "subtotal gastrectomy" where gastrointestinal continuity after the resection was attained with an anastomosis between the stomach and the duodenum, a gastroduodenostomy.
The procedure was originally performed as a way to resect peptic ulcers caused by hyperacidity. Billroth removed up to 70% of the stomach. Modern variations of the procedure are less agressive, resecting only 50% of the distal stomach (a hemigastrectomy), or an antrectomy.
After Billroth's pioneering work, several variations on the procedure appeared (Polya, Hofmeister) as well as different techniques (open vs. laparoscopic), and the use of different materials, starting with carbolized silk to the modern endolaparoscopic surgical staplers.
The accompanying image shows the digestive tract before the resection. The area to the resected (specimen) is grayed out. If you hover your cursor over the image you will see the completed Billroth I procedure.
In the completed procedure you can see A: The stapled-closed proximal gastric pouch. B: The duodenum. The red arrow points to the gastroduodenostomy, that is, the anastomosis between the stomach and the duodenum which in this case was done in the posterior aspect of the proximal gastric pouch. Bear in mind that this sketch depicts only one of the many ways of performing this procedure
Images property of: CAA.Inc. Artist:Dr. E. Miranda
- Details
This article is part of the series "A Moment in History" where we honor those who have contributed to the growth of medical knowledge in the areas of anatomy, medicine, surgery, and medical research.

Original image courtesy of the
National Library of Medicine
Jean Louis Petit (1674 – 1750). French surgeon and anatomist, Jean Louis Petit was born in Paris in on March 13, 1674. His family rented an apartment at his house to Alexis Littre (1658 – 1726), a French anatomist. Petit became an apprentice of Littre at seven years of age, helping him in the dissections for his lectures and at an early age became the assistant in charge of the anatomic amphitheater.
Because of Petit’s dedication to anatomy and medicine, in 1690 at the age of sixteen, became a disciple of a famous Paris surgeon, Castel.
In 1692, Petit entered the French army and performed surgery in two military campaigns. By 1693 he started delivering lectures and was accepted as a great surgeon, being invited to the most difficult operations. In 1700 he was appointed Chief Surgeon of the Military School in Paris and in the same year he received the degree of Master of Surgery from the Faculty of Paris.
In 1715 he was made a member of the Royal Academy of Sciences and an honorary member of the Royal Society of London. He was appointed by the King as the first Director General of the Royal Academy of Surgery when it was founded in 1731.
Petit’s written works are of historical importance. “Traite des Maladies des Os” ( A Treatise on Bone Diseases); “Traite des Maladies Chirurgicales et des Operation” (A Treatise on Surgical Diseases and their Operations” This last book was published posthumously in 1774. He also published a monograph on hemorrhage, another on lachrymal fistula, and others.
He was one of the first to perform choIecystotomy and mastoidotomy. His original tourniquet design for amputations saved many in the battlefield and the design of the same surgical instrument today has not changed much since its invention by him.
His name is remembered in the lumbar triangle, also called the "triangle of Petit", and the abdominal hernia that can ensue through that area of weakness, the lumbar hernia or "Petit's hernia".
Sources:
1. “Jean Louis Petit – A Sketch of his Life, Character, and Writings” Hayne, AP San Fran Western Lancet 1875 4: 446-454
2. “Oeuvres compl?tes de Jean-Louis Petit” 1837 Imprimerie de F. Chapoulaud
3. Extraits de l'eloge de Jean-Louis Petit Ius dans Ia seance publique de I' Academie royale de chirurgie du 26 mai 1750” Louis A. Chirurgie 2001: 126 : 475- 81
- Details
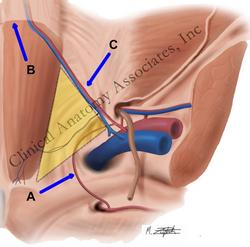
Important for inguinal hernia anatomy and surgery, this term is Latin from [corona] meaning "crown' and [mortis] meaning "death'; the "crown or circle of death". The corona mortis (blue arrow) refers to an anatomical variation1, a vascular anastomosis between the obturator and the external iliac vascular systems that passes over Cooper's pectineal ligament and posterior to the lacunar (Gimbernat's) ligament.
In some cases, the corona mortis is the actual obturator artery that arises from the inferior epigastric artery instead of the internal iliac artery. It can also arise from the external iliac artery. In both cases, it has been called an "aberrant obturator artery". This could be a misnomer, as this anatomical variation can be present in up to 25% of the cases. When present, the corona mortis can be injured when a surgeon looks to enlarge the femoral ring by opening the lacunar ligament from the anterior aspect. In this approach the "corona mortis" is not visible, as it is found immediately posterior to the lacunar ligament. This vascular structure could even be endangered in a laparoscopic procedure for inguinal of femoral hernia repair and a staple or tack is driven blindly into the pectineal (Cooper's) ligament.
Berberoglu states that "although these tiny anastomoses... have been described in classical anatomy textbooks, these texts neglect to mention that theses anastomoses can be life-threatening".
In some rare cases, the corona mortis (aberrant obturator artery) coexists with the normal obturator artery. Although called a [corona], this anatomical structure is an incomplete circle. In the image, the [corona mortis] is labeled "A".
Sources:
1. Rusu et al: "Anatomical considerations on the corona mortis" Surg Radiol Anat (2010) 32:17–24
2. Berberoglu et al: "An anatomic study in seven cadavers and an endoscopic study in 28 patients" Surg Endosc (2001) 15:72-75
Image property of:CAA.Inc.. Artist:M. Zuptich
- Details
UPDATED: The word [catamenial] is Greek. The prefix [cata-] arises from [, from [κάτω] (kato) meaning "down", "down because of", or "down to", the root term )[-men-] from [μήνας] (menas) meaning "month", referring to "lunar month" or to a female's menstrual cycle, which is usually just about a lunar month long, and the adjectival suffix [-ial] means "pertaining to".
[Catamenial] then means "to be down (sick) during a menstrual cycle" and refers to a condition that recurs in reference to menses.
Examples of the use of this word are:
• Catamenial depression or catamenial psychosis
• Catamenial pneumothorax - related to endometriosis
• Catamenial epilepsy or seizures
The links will open scholarly articles that use this word.
- Details
The root term [-asthen-] originates from the Greek word [ασθενεσ] (asthenes), meaning “weak” or “feeble”. It can be used with the adjectival suffixes [-ic] or [-ia], both meaning “pertaining to” to form the medical words [asthenic] and [asthenia], meaning “weak” and “weakness”.
It is also found in other medical words such as:
- Myasthenia: The root term [-my-] means “muscle”. Weak muscles
- Neurasthenia: The root term [-neur-] means “nerve”. Initially used to denote an actual weak nerve, it has evolved today to mean someone with a “weak nerves condition”, with fatigue, headaches or migraines, and sometimes depression.
- Angiasthenia or angioasthenia: Both are correct. The root term [-angi-] means “vessel”. The terms refer to a weak condition of the cardiovascular system.
- Asthenophobia: Fear of being weak
Personal note: There was a time in the 1800’s when the term [asthenic] was used to refer to a person as a “weakling”.
- Details
The root term [-pyr] originates from the Greek [πυροσ] (pyros) meaning “fire”. In medical terminology it is used in reference to high temperature or “fever” as in the following terms:
- Antipyretic: The prefix [anti-] means “against”. A medicine that reduces fever
- Apyretic: No fever
- Pyrexia: Condition of fever. Fever
- Pyretic: That which can cause fever
- Pyrogenic: The suffix [-(o)genic] means “generation” or “cause”. Something that can generate fever
- Pyrolytic: The suffix [-(o)lytic] means “destruction” or “dissolution”. Something that destroys or stops fever
- Pyromaniac: An individual obsessed by fire
The term can also be found in vernacular English is words such as:
- Pyrotechnics: Fireworks
- Pyromancy: The art of divination by the observation of fire