Medical Terminology Daily (MTD) is a blog sponsored by Clinical Anatomy Associates, Inc. as a service to the medical community. We post anatomical, medical or surgical terms, their meaning and usage, as well as biographical notes on anatomists, surgeons, and researchers through the ages. Be warned that some of the images used depict human anatomical specimens.
You are welcome to submit questions and suggestions using our "Contact Us" form. The information on this blog follows the terms on our "Privacy and Security Statement" and cannot be construed as medical guidance or instructions for treatment.
We have 509 guests online

Jean George Bachmann
(1877 – 1959)
French physician–physiologist whose experimental work in the early twentieth century provided the first clear functional description of a preferential interatrial conduction pathway. This structure, eponymically named “Bachmann’s bundle”, plays a central role in normal atrial activation and in the pathophysiology of interatrial block and atrial arrhythmias.
As a young man, Bachmann served as a merchant sailor, crossing the Atlantic multiple times. He emigrated to the United States in 1902 and earned his medical degree at the top of his class from Jefferson Medical College in Philadelphia in 1907. He stayed at this Medical College as a demonstrator and physiologist. In 1910, he joined Emory University in Atlanta. Between 1917 -1918 he served as a medical officer in the US Army. He retired from Emory in 1947 and continued his private medical practice until his death in 1959.
On the personal side, Bachmann was a man of many talents: a polyglot, he was fluent in German, French, Spanish and English. He was a chef in his own right and occasionally worked as a chef in international hotels. In fact, he paid his tuition at Jefferson Medical College, working both as a chef and as a language tutor.
The intrinsic cardiac conduction system was a major focus of cardiovascular research in the late nineteenth and early twentieth centuries. The atrioventricular (AV) node was discovered and described by Sunao Tawara and Karl Albert Aschoff in 1906, and the sinoatrial node by Arthur Keith and Martin Flack in 1907.
While the connections that distribute the electrical impulse from the AV node to the ventricles were known through the works of Wilhelm His Jr, in 1893 and Jan Evangelista Purkinje in 1839, the mechanism by which electrical impulses spread between the atria remained uncertain.
In 1916 Bachmann published a paper titled “The Inter-Auricular Time Interval” in the American Journal of Physiology. Bachmann measured activation times between the right and left atria and demonstrated that interruption of a distinct anterior interatrial muscular band resulted in delayed left atrial activation. He concluded that this band constituted the principal route for rapid interatrial conduction.
Subsequent anatomical and electrophysiological studies confirmed the importance of the structure described by Bachmann, which came to bear his name. Bachmann’s bundle is now recognized as a key determinant of atrial activation patterns, and its dysfunction is associated with interatrial block, atrial fibrillation, and abnormal P-wave morphology. His work remains foundational in both basic cardiac anatomy and clinical electrophysiology.
Sources and references
1. Bachmann G. “The inter-auricular time interval”. Am J Physiol. 1916;41:309–320.
2. Hurst JW. “Profiles in Cardiology: Jean George Bachmann (1877–1959)”. Clin Cardiol. 1987;10:185–187.
3. Lemery R, Guiraudon G, Veinot JP. “Anatomic description of Bachmann’s bundle and its relation to the atrial septum”. Am J Cardiol. 2003;91:148–152.
4. "Remembering the canonical discoverers of the core components of the mammalian cardiac conduction system: Keith and Flack, Aschoff and Tawara, His, and Purkinje" Icilio Cavero and Henry Holzgrefe Advances in Physiology Education 2022 46:4, 549-579.
5. Knol WG, de Vos CB, Crijns HJGM, et al. “The Bachmann bundle and interatrial conduction” Heart Rhythm. 2019;16:127–133.
6. “Iatrogenic biatrial flutter. The role of the Bachmann’s bundle” Constán E.; García F., Linde, A.. Complejo Hospitalario de Jaén, Jaén. Spain
7. Keith A, Flack M. The form and nature of the muscular connections between the primary divisions of the vertebrate heart. J Anat Physiol 41: 172–189, 1907.
"Clinical Anatomy Associates, Inc., and the contributors of "Medical Terminology Daily" wish to thank all individuals who donate their bodies and tissues for the advancement of education and research”.
Click here for more information
- Details
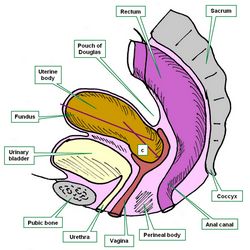
The word [trachelectomy] is composed of the root term [-trache-] which arises from the Greek word [τράχηλος] (trahelos), meaning “neck”, and the suffix [-ectomy] meaning “removal of”. The word [trachelectomy] then means “removal of the neck”.
Another way to refer to this procedure is [cervicectomy], where the root term [-cervic-] arises fron the Latin term [cervix], also meaning neck.
The procedure refers to the removal of the neck or cervix of the uterus. It can be performed as a procedure where the cervix is removed leaving the body of the uterus or [uterus proper] in place. This is done is younger females where there is a cervical cancer, but there is still the possibility of attaining pregnancy. The procedure carries a higher chance of miscarriage and the baby must be delivered via a Cesarean section.
A second reason to remove the cervix of the uterus is as a secondary procedure, after the uterus proper has been removed as part of a supracervical hysterectomy and the cervix, left behind, shows signs of cancer.
Medical terminology note: Trachelectomy and cervicectomy… why are there two terms for the same procedure? That is actually quite common in medical terminology, where you have words having the same meaning that arise from Latin and Greek. In fact, there are cases where there are more than two terms for the same organ or procedure, and let’s not count the vernacular terms on top! This makes medical terminology and interesting and fascinating topic. I would suggest that you click around the links for this article, you will find some interesting information. Dr. Miranda
- Details
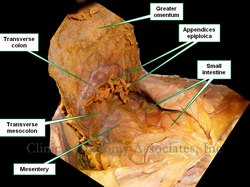
UPDATED: The term [mesentery] is of Greek origin. The prefix [mes(o)-] arises from the Greek [μέσο] meaning "middle", the root term [-enter-] means "small intestine" or "intestine", and the suffix [-y] means "process" or "structure". Thus, the mesentery is "a structure in the middle".
The term [mesentery] can be used as a generic word to denote a double-layered peritoneal membrane that stretches between an abdominal viscus and the abdominal wall. A more precise use of the term is that of mesentery proper, which extends between the posterior abdominal wall and the jejunum and ileum. The superior mesenteric artery and veins are found at the root of the mesentery proper, along with a large accumulation of lymphatic nodes, and sympathetic and parasympathetic nerves.
Between the two layers of the mesentery proper, there are jejunal and ileal arteries and veins, a complex system of arterial and venous arches, as well as lymphatic vessels, autonomic nerves, and varying degrees of fat. Because of the presence of the mesentery proper, the jejunum and ileum are mobile or intraperitoneal, that is, they can slither, turn and twist with the movements of peristalsis. This movement is helped by the presence of a small amount of peritoneal fluid.
The fact that the mesentery is intraperitoneal is important in surgery. If the organ can already move around because of its mesentery, then it does not need to be "mobilized", it is already mobile!! If the organ (jejunum or ileum) have adhesions that limit their mobility within the abdominal cavity, the surgeon may have to perform and adhesiolysis to restore their mobility.
The first image shows an anatomical dissection where the greater omentum has been pulled anteriorly, exposing the small intestine and its mesentery, as well as the transverse mesocolon. Click on the image for a larger depiction. The second image (courtesy of Dr. Michiaki Akashi) is artwork depicting the surgical technique of transillumination, where the surgeon will shine a light through the mesentery to visualize the blood supply to the intestine prior to ligation and transection. The mesentery-like structure being transilluminated is the transverse mesocolon
WARNING: The first image is a photograph of a human dissection and can be considered descriptive.
NOTE: My personal thanks to Michiaki Akashi, M.D.for allowing us to use his artwork in this article. Dr. Akashi works as a surgeon and pathologist in the Saga Prefectural Hospital Koseikan in Saga, Japan.Dr. Miranda
First image property of: CAA.Inc. Photographer: David M. Klein
- Details
UPDATED: The suffix [-(o)megaly] means "enlargement". It is related to the root term [-megal-], which is a derivate of the Greek word [μεγάλος] (megalos), meaning "large" or "big". The suffix component [-y] means "process". Usually used to refer to the abnormal or pathological enlargement of an organ.
Some applications of this suffix are:
- Cardiomegaly: Enlargement of the heart
- Splenomegaly: Enlargement of the spleen
- Lienomegaly: Enlargement of the spleen. the root term [-lien-] also means "spleen"
- Acromegaly: From the Greek prefix [acro-], meaning "top" or "extremity". Enlargement of the face, hands, and feet, caused by dysfunction of the hypophysis
- Hepatomegaly: Enlargement of the liver
Note: The links to Google Translate include an icon that will allow you to hear the Greek or Latin pronunciation of the word.
Thanks to our contributor Dr. Sanford Osher for inspiring this update.
- Details
The prefix (sometimes used as a root term) [hydr-] has a Greek origin [υδωρο], meaning "water". It can be found in many common and scientific terms such as "hydrostatic", "hydroelectric", and "hydroplaning". It is also used in medical terms such as:
- Hydrocephalus: Literally "water in the head". Refers to a pathology where there is excess cerebrospinal fluid in the ventricular system of the brain
- Hydrocele: The suffix [-(o)cele] means "bulge" or "hernia". A watery mass or bulge, usually found in the scrotum.
- Hydrops or hydropsy: The excessive accumulation of serous fluid in a body cavity, such as ascites.
- Hydramnios: Excessive accumulation of fluid in the amniotic cavity during pregnancy
- Details
This article is part of the series "A Moment in History" where we honor those who have contributed to the growth of medical knowledge in the areas of anatomy, medicine, surgery, and medical research.
Giulio Cesare Aranzio (1530 -1589) Italian surgeon and anatomist. Born in Bologna, Giulio Cesare Aranzio is better known by the Latinized version of his name Julius Caesar Arantius. His Italian last name is sometimes spelled Aranzi.
Born in a poor family, Aranzio began his medical studies under the tutelage of his uncle, Bartolommeo Maggi (1477 – 1552), studied medicine at the University of Bologna where he graduated MD in 1556. The same year he became a Professor of Anatomy and Surgery at the in 1556. Arantius was the first lecturer at the University of Bologna to hold a separate professorship of anatomy. Before him, the University would allow any surgeon to perform dissection and lectures.
Arantius had several publications that include:
• Observationes Anatomicas (Anatomical Observations)
• De Humano Foetu Opusculum (On the Human Fetus)
• De Tumoribus Secundum Locos Affectos (Tumors according to the affected places)
• Hippocratis librum de vulneribus capitis commentarius brevis (Short commentary on Hippocrates’ book on head wounds)
Arantius was the first to describe the foramen ovale (fossa ovalis) and the ductus arteriosus, discoveries that were later erroneously ascribed to Leonardo Bottalus (Botal). He also described the nodules in the leaflets of the aortic valve that today bear his name (nodules of Arantius) which he described as being “cartilaginous” in nature. This is not as farfetched as it seems as these nodules can become hypertrophic and harden with age. Arantius was also the first to describe the hippocampus, a formation on the brain associated with the limbic system, mood disorders, and depression.
Arantius was a consummate anatomist and a great surgeon. Apparently he treated nasal polyps, performed nasal reconstructions and a number of surgeries ahead of his time. One of his great anatomical observations was that the blood in the heart did not pass through “invisible pores” in the interventricular septum, but rather exits the heart through the pulmonary trunk, setting the stage for the discovery of circulation by William Harvey (1578 – 1609)
We have not been able to find a portrait of Arantius and the only reference is a a bust with the name “Aranzio” located at the Biblioteca comunale dell'Archiginnasio in Bologna, Italy. The bust is found in the anatomical amphitheater, built in 1637. Unfortunately, the theater was severly damaged in January 29, 1944 during WWII. It has been meticulously restored over the years. Here is an article (in Italian) on the amphitheater.
Sources:
1. “Giulio Cesare Arantius (1530-1589): a surgeon and anatomist: his role in nasal reconstruction and influence on Gaspare Tagliacozzi” . Gurunluoglu R, Gurunluoglu A Ann Plast Surg. 2008 Jun;60(6):717-22
2. “Giulio Cesare Aranzio (Arantius) (1530-89) in the pageant of anatomy and surgery” Gurunluoglu R, Shafighi M, Gurunluoglu A, Cavdar S. J Med Biogr. 2011 May;19(2):63-9
3. “Hippocampus – Why is it studied so frequently?” Radonjic, V. et al Vojnosanit Pregl 2014; 71(2): 195–201
4: “The history of Bologna University's Medical School over the centuries, A Short Review” Moroni, P. Acta Dermatoven APA Vol 9, 2000, No 2 73-75
- Details
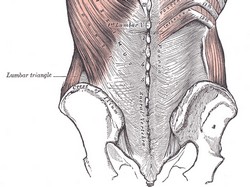
The [lumbar triangle] is a well-defined triangular space in the posterolateral lumbar region. Also known as the inferior lumbar triangle, its boundaries are: inferior, the iliac crest; anteromedial: latissimus dorsi muscle; posterolateral: posterior border of the external oblique muscle. The triangle has a superior apex, and the floor of the triangle is the internal oblique muscle.
The triangle is named after Jean-Louis Petit (1674 - 1750), a French Surgeon who is said to have been an anatomy teacher at an early age and became a surgeon when he was only eighteen!
The lumbar triangle is an area that is not as thick as the rest of the abdominal wall and as such it is a site of potential weakness that can lead to a lumbar hernia, also known as Petit’s hernia.
Sources:
1. “Jean Louis Petit – A Sketch of his Life, Character, and Writings” Hayne, AP San Fran Western Lancet 1875 4: 446-454
2. “Oeuvres compl?tes de Jean-Louis Petit” 1837 Imprimerie de F. Chapoulaud
3. Extraits de l'eloge de Jean-Louis Petit Ius dans Ia seance publique de I' Academie Royale de Chirurgie du 26 mai 1750” Louis A. Chirurgie 2001: 126 : 475- 81