Medical Terminology Daily (MTD) is a blog sponsored by Clinical Anatomy Associates, Inc. as a service to the medical community. We post anatomical, medical or surgical terms, their meaning and usage, as well as biographical notes on anatomists, surgeons, and researchers through the ages. Be warned that some of the images used depict human anatomical specimens.
You are welcome to submit questions and suggestions using our "Contact Us" form. The information on this blog follows the terms on our "Privacy and Security Statement" and cannot be construed as medical guidance or instructions for treatment.
We have 512 guests online

Jean George Bachmann
(1877 – 1959)
French physician–physiologist whose experimental work in the early twentieth century provided the first clear functional description of a preferential interatrial conduction pathway. This structure, eponymically named “Bachmann’s bundle”, plays a central role in normal atrial activation and in the pathophysiology of interatrial block and atrial arrhythmias.
As a young man, Bachmann served as a merchant sailor, crossing the Atlantic multiple times. He emigrated to the United States in 1902 and earned his medical degree at the top of his class from Jefferson Medical College in Philadelphia in 1907. He stayed at this Medical College as a demonstrator and physiologist. In 1910, he joined Emory University in Atlanta. Between 1917 -1918 he served as a medical officer in the US Army. He retired from Emory in 1947 and continued his private medical practice until his death in 1959.
On the personal side, Bachmann was a man of many talents: a polyglot, he was fluent in German, French, Spanish and English. He was a chef in his own right and occasionally worked as a chef in international hotels. In fact, he paid his tuition at Jefferson Medical College, working both as a chef and as a language tutor.
The intrinsic cardiac conduction system was a major focus of cardiovascular research in the late nineteenth and early twentieth centuries. The atrioventricular (AV) node was discovered and described by Sunao Tawara and Karl Albert Aschoff in 1906, and the sinoatrial node by Arthur Keith and Martin Flack in 1907.
While the connections that distribute the electrical impulse from the AV node to the ventricles were known through the works of Wilhelm His Jr, in 1893 and Jan Evangelista Purkinje in 1839, the mechanism by which electrical impulses spread between the atria remained uncertain.
In 1916 Bachmann published a paper titled “The Inter-Auricular Time Interval” in the American Journal of Physiology. Bachmann measured activation times between the right and left atria and demonstrated that interruption of a distinct anterior interatrial muscular band resulted in delayed left atrial activation. He concluded that this band constituted the principal route for rapid interatrial conduction.
Subsequent anatomical and electrophysiological studies confirmed the importance of the structure described by Bachmann, which came to bear his name. Bachmann’s bundle is now recognized as a key determinant of atrial activation patterns, and its dysfunction is associated with interatrial block, atrial fibrillation, and abnormal P-wave morphology. His work remains foundational in both basic cardiac anatomy and clinical electrophysiology.
Sources and references
1. Bachmann G. “The inter-auricular time interval”. Am J Physiol. 1916;41:309–320.
2. Hurst JW. “Profiles in Cardiology: Jean George Bachmann (1877–1959)”. Clin Cardiol. 1987;10:185–187.
3. Lemery R, Guiraudon G, Veinot JP. “Anatomic description of Bachmann’s bundle and its relation to the atrial septum”. Am J Cardiol. 2003;91:148–152.
4. "Remembering the canonical discoverers of the core components of the mammalian cardiac conduction system: Keith and Flack, Aschoff and Tawara, His, and Purkinje" Icilio Cavero and Henry Holzgrefe Advances in Physiology Education 2022 46:4, 549-579.
5. Knol WG, de Vos CB, Crijns HJGM, et al. “The Bachmann bundle and interatrial conduction” Heart Rhythm. 2019;16:127–133.
6. “Iatrogenic biatrial flutter. The role of the Bachmann’s bundle” Constán E.; García F., Linde, A.. Complejo Hospitalario de Jaén, Jaén. Spain
7. Keith A, Flack M. The form and nature of the muscular connections between the primary divisions of the vertebrate heart. J Anat Physiol 41: 172–189, 1907.
"Clinical Anatomy Associates, Inc., and the contributors of "Medical Terminology Daily" wish to thank all individuals who donate their bodies and tissues for the advancement of education and research”.
Click here for more information
- Details
The anatomical term [crista terminalis] is Latin. [Crista] refers to the crest of a helmet, a tuft (of hair or feathers), or a ridge. The word [terminalis] means "end" or "terminal". The term then means "the terminal or end ridge".
The crista terminalis is a superoinferior muscular ridge found in the right atrium marking the boundary between the smooth wall of the right atrium, also known as the "sinus venarum" (venous sinus), and the muscular wall of the right atrial appendage. The muscular wall of the right atrial appendage is comb-shaped and is called the pectinate muscle.
Because of the longitudinal direction of the muscular fibers of the crista terminalis, it is considered to be one of the pathways for electrical transmission of the cardiac depolarization between the sinoatrial (SA) node and the atrioventricular (AV) node.
The crista terminalis causes a superoinferior longitudinal depression on the surface of the heart known as the sulcus terminalis.
The accompanying image is a dissection of a human heart and shows the crista terminalis, pectinate muscle, fossa ovalis, the ostium of the coronary sinus, the right atrial smooth wall of the sinus venarum. Click on the image for a larger version. The animated image does a slow pass trough all these and other structures.
Sources:
1. "The origin of Medical Terms" Skinner, AH, 1970
2. "Terminologia Anatomica: International Anatomical Terminology (FCAT)" Thieme, 1998
3. "Tratado de Anatomia Humana" Testut et Latarjet 8th Ed. 1931 Salvat Editores, Spain
Image courtesy of Rocky Vista University,College of Osteopathic Medicine, Parker, CO
- Details
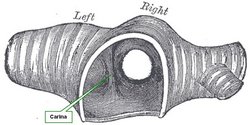
The word [carina] is Greek, from [καρίνα] meaning “keel”, as in the keel of a boat.
The carina is an anteroposterior elevation found at the point of bifurcation of the trachea into the left and right bronchi. When looking at it from the superior aspect, it does look as if you were looking at the keel of boat from the bottom up, and this is the image that endoscopists see when looking at this area. See the accompanying image.
The bifurcation of the trachea and the carina are usually found at the level of the sternal angle (of Louis), which is about the level of the superior border of the 5th thoracic vertebra.
Since the right bronchus is slightly wider than the left bronchus, the carina is usually slightly displaced to the left of the midline.
The lymph nodes that surround the area of the bifurcation of the trachea, and inferior to the bifurcation are called the carinal nodes.
- Details
Although not a medical term per se, we use the word [vernacular] constantly on this blog to refer to terms used commonly or colloquially by non-health care professionals.
Merriam-Webster’s definitions of [vernacular] are multiple, all pointing to common usage by a group:
• of, relating to, or using the language of ordinary speech rather than formal writing
• of, or relating to the common style of a particular time, place, or group
• using a language or dialect native to a region or country rather than a literary, cultured, or foreign language
• of, relating to, or being a nonstandard language or dialect of a place, region, or country
• of, relating to, or being the normal spoken form of a language
• applied to a plant or animal in the common native speech as distinguished from the Latin nomenclature of scientific classification
This last definition is the one that applies mostly to what we mean in this blog. While we may use the anatomical term “rectus abdominis” , most people would say “six-pack” – which is wrong on two aspects: it is vernacular, and it is not a “six pack”, if you count them, you will see that a well-developed rectus abdominis has eight bellies, four on each side, making it really an “eight pack”!
Another one would be the vernacular term "pinky" to refer to the fifth digit of the hand. Yet another one would be the use of the vernacular term “stomach” to refer to the abdomen, that is one of my pet peeves!
- Details
UPDATED: The word [hypochondriac] is formed by the prefix [hypo-], meaning "below", the root term [-chondr-], meaning "cartilage", and the adjectival suffix [-iac], meaning "pertaining to". A literal translation would be "pertaining to (the area) below the cartilage"; this does nothing to explain what we understand as a "hypochondriac" patient.
The word [hypochondrium], was first used by Hippocrates of Cos (460 BC - 370 BC) to denote the anterior bilateral areas below the lower costal cartilages of the thorax, what we known today as two of the abdominal regions, the hypochondriac regions.
These two areas contain on the right, the liver and gallbladder, and on the left, the spleen, part of the stomach, and the left flexure of the colon. Because of the visceral sensations referred by some patients in these areas without any apparent problems, these symptoms started to be called "hypochondriac symptoms". It did not take much time to refer to a patient that refers pathological symptoms without being sick as an "hypochondriac". The first one to actually use this term in a publication was Robert Whytt (1714 - 1766), a Scottish physician.
- Details
This article is part of the series "A Moment in History" where we honor those who have contributed to the growth of medical knowledge in the areas of anatomy, medicine, surgery, and medical research.

Don Antonio de Gimbernat i Arbos
UPDATED: Don Antonio de Gimbernat y Arbós (1734-1816). Spanish anatomist and surgeon. His complete name was Don Manuel Luis Antonio de Gimbernat y Arbós. He was born to a farmer’s family in 1734 in Cambrils (Tarragona), in what today is Cataluña. Gimbernat studied Latin and Philosophy at the University of Cervera, continuing his studies at the School of Surgery in Cádiz, where he graduated in 1762.
Gimbernat joined the Spanish Navy, but because of this capabilities, in 1765 he was offered the position of Anatomy Professor at the Royal School of Surgery in Barcelona. In 1768 he made an anatomical discovery that would render him immortal: he demonstrated the presence of the lacunar ligament. Furthermore he applied his knowledge of this ligament to improve on the surgical technique to reduce a strangulated femoral hernia. Gimbernat also discovered the lymph node found deep in the femoral ring (later to be known as Cloquet’s or Rosenmueller’s node)
In 1774 Gimbernat traveled through Europe to learn the latest surgical techniques. This trip was sponsored by King Carlos III. During his stay in London Gimbernat studied with John Hunter (1728 – 1793). In an attitude not common for a student at the time, at the end of one of Hunter's anatomical lectures on hernia, Gimbernat asked to go to the cadaver and demonstrate his findings. With approval of the teacher, he demonstrated for Hunter the lacunar ligament as well as his strangulated femoral hernia technique. Hunter watched the demonstration and at the end of it he just said "You are correct, sir".
Hunter was so impressed that from that day on he referred to the lacunar ligament as “Gimbernat’s ligament" and adopted his surgical technique. Gimbernat also showed Hunter his studies and technique to repair diaphragmatic hernias.
Manuel Gimbernat participated in the creation of the Spanish Royal School of Surgery, became a professor of surgery and orthopedics, and in 1789 he was named First Royal Surgeon and president of all the surgical schools in Spain.
In 1793, Gimbernat published his “ Nuevo Método de Operar en la Hernia Crural” dedicated to King Charles IV, which was translated as “A New Method of Operating for the Femoral Hernia”, into English in 1795.
In 1803 the Spanish king Carlos IV commissioned Don Francisco Javier de Balmis i Berenguer (1753 – 1819), a Spanish physician, to find a solution to the smallpox problem in the Spanish colonies in South America. While planning what was later to be known as the “Royal Philanthropic Vaccine Expedition” Balmis received critical contributions from Don Manuel Gimbernat.
All of his titles and positions were removed by King Fernando VII because Gimbernat was a supporter of Napoleon during his invasion of Spain in 1808. Sick, poor, blind, and with ailing mental faculties, Don Manuel Gimbernat died in Madrid on November 17, 1816.
Gimbernat was also a pioneer in ophthalmology, vascular surgery and urology. As for his incredible anatomical dissection capabilities, Gimbernat often said “mi autor más favorito es el cadaver humano" (my favorite author is the human body”
Personal note: My thanks to Dr. José Luis Bueno-López for his correction of the name of Gimbernat: "Although don Antonio de Gimbernat y Arbós was born in a town in Catalonia, Spain, he never wrote his name nor his contemporaries did, with the particle 'i' between his two family names (in the manner of the Catalan language) but with particle 'y' in the way of the Spanish language". There are many articles where Gimbernat's last name is written "Gimbernat i Arbos" (see link #3 on the Source section) which according to Dr. Bueno-López is incorrect. To read the article co-authored by Dr. Bueno-López on Gimbernat (#6 in our Sources section) click here.
Sources:
1. “Manuel Antonio de Gimbernat y Arbós. 1734-1816” Trauma (2012) 23: (1)
2. ” Gimbernat y Arbós, Antonio de (1734-1816) Loukas M et al World J Surg 2007; 31: 855-7
3. “Epónimos médicos: Ligamento de Gimbernat” Febrer JLF 1999 (Link)
4. “Antonio de Gimbernat (1734- 1816). Anatomist and surgeon” Puig-LaCalle J, Mart?-Pujol R. Arch Surg 1995; 130: 1017- 20
5. “Antonio de Gimbernat, 1734-1816” Matheson NM. Proc R Soc Med 1949; 42: 407-10.
6. "Antonio Gimbernat y Arbós: An Anatomist-surgeon of the Enlightenment (In the 220th Anniversary of his ‘‘A New Method of Operating the Crural Hernia’" Arraez-Aybar LA, Bueno-Lopez JL. Clin Anat (2013) 26:800–809
- Details
The [subarachnoid space] is the region or interval found between the deeply situated pia mater and the more superficial arachnoid mater. Extending between these two layers there is a fine meshwork or trabeculae of connective tissue strand. Also, between these two layers we find the CSF or cerebrospinal fluid. The subarachnoid space extends all around the brain and the spinal cord.
Where these two layers are in almost direct contact or apposition, the subarachnoid space is small, but there are areas deep in the sulci of the brain, where there can be slightly larger spaces. In fact, there are specific areas of the brain where the subarachnoid space is large enough (with consequent larger accumulations of CSF) that these areas are know as subarachnoid cisterns.
At the level of the posterior and lateral aspects of the medulla oblongata the subarachnoid space has communications with the internal cavities of the brain known as the ventricular system. The cerebrospinal fluid is produced deep within the ventricular system in a series of structures known as the choroid plexuses.