Medical Terminology Daily (MTD) is a blog sponsored by Clinical Anatomy Associates, Inc. as a service to the medical community. We post anatomical, medical or surgical terms, their meaning and usage, as well as biographical notes on anatomists, surgeons, and researchers through the ages. Be warned that some of the images used depict human anatomical specimens.
You are welcome to submit questions and suggestions using our "Contact Us" form. The information on this blog follows the terms on our "Privacy and Security Statement" and cannot be construed as medical guidance or instructions for treatment.
We have 1121 guests online

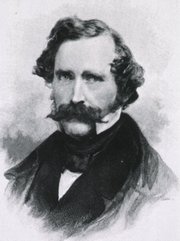
Jean George Bachmann
(1877 – 1959)
French physician–physiologist whose experimental work in the early twentieth century provided the first clear functional description of a preferential interatrial conduction pathway. This structure, eponymically named “Bachmann’s bundle”, plays a central role in normal atrial activation and in the pathophysiology of interatrial block and atrial arrhythmias.
As a young man, Bachmann served as a merchant sailor, crossing the Atlantic multiple times. He emigrated to the United States in 1902 and earned his medical degree at the top of his class from Jefferson Medical College in Philadelphia in 1907. He stayed at this Medical College as a demonstrator and physiologist. In 1910, he joined Emory University in Atlanta. Between 1917 -1918 he served as a medical officer in the US Army. He retired from Emory in 1947 and continued his private medical practice until his death in 1959.
On the personal side, Bachmann was a man of many talents: a polyglot, he was fluent in German, French, Spanish and English. He was a chef in his own right and occasionally worked as a chef in international hotels. In fact, he paid his tuition at Jefferson Medical College, working both as a chef and as a language tutor.
The intrinsic cardiac conduction system was a major focus of cardiovascular research in the late nineteenth and early twentieth centuries. The atrioventricular (AV) node was discovered and described by Sunao Tawara and Karl Albert Aschoff in 1906, and the sinoatrial node by Arthur Keith and Martin Flack in 1907.
While the connections that distribute the electrical impulse from the AV node to the ventricles were known through the works of Wilhelm His Jr, in 1893 and Jan Evangelista Purkinje in 1839, the mechanism by which electrical impulses spread between the atria remained uncertain.
In 1916 Bachmann published a paper titled “The Inter-Auricular Time Interval” in the American Journal of Physiology. Bachmann measured activation times between the right and left atria and demonstrated that interruption of a distinct anterior interatrial muscular band resulted in delayed left atrial activation. He concluded that this band constituted the principal route for rapid interatrial conduction.
Subsequent anatomical and electrophysiological studies confirmed the importance of the structure described by Bachmann, which came to bear his name. Bachmann’s bundle is now recognized as a key determinant of atrial activation patterns, and its dysfunction is associated with interatrial block, atrial fibrillation, and abnormal P-wave morphology. His work remains foundational in both basic cardiac anatomy and clinical electrophysiology.
Sources and references
1. Bachmann G. “The inter-auricular time interval”. Am J Physiol. 1916;41:309–320.
2. Hurst JW. “Profiles in Cardiology: Jean George Bachmann (1877–1959)”. Clin Cardiol. 1987;10:185–187.
3. Lemery R, Guiraudon G, Veinot JP. “Anatomic description of Bachmann’s bundle and its relation to the atrial septum”. Am J Cardiol. 2003;91:148–152.
4. "Remembering the canonical discoverers of the core components of the mammalian cardiac conduction system: Keith and Flack, Aschoff and Tawara, His, and Purkinje" Icilio Cavero and Henry Holzgrefe Advances in Physiology Education 2022 46:4, 549-579.
5. Knol WG, de Vos CB, Crijns HJGM, et al. “The Bachmann bundle and interatrial conduction” Heart Rhythm. 2019;16:127–133.
6. “Iatrogenic biatrial flutter. The role of the Bachmann’s bundle” Constán E.; García F., Linde, A.. Complejo Hospitalario de Jaén, Jaén. Spain
7. Keith A, Flack M. The form and nature of the muscular connections between the primary divisions of the vertebrate heart. J Anat Physiol 41: 172–189, 1907.
"Clinical Anatomy Associates, Inc., and the contributors of "Medical Terminology Daily" wish to thank all individuals who donate their bodies and tissues for the advancement of education and research”.
Click here for more information
- Details
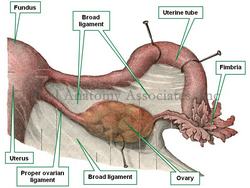
The root term [-salping-] arises from the Greek [σάλπιγγα] or [salpinx], meaning "trumpet" or "bugle". Because of their trumpet shape, there are two anatomical structures where this term applies, one is the uterine or Fallopian tube, and the other is the auditory or Eustachian tube.
This root term is used in medical terms such as:
- Salpingitis: An inflammation or infection of the Fallopian (uterine) tube
- Salpingectomy: Removal of one or both Fallopian tubes
- Salpingopharyngeus: A muscle that extends between the Eustachian (auditory) tube and the pharynx
- Salpingooophorectomy: This combined root term adds the root [-oophor-] meaning ovary. The suffix [-ectomy] means "removal". The removal of the uterine tubes and the ovaries. This operation can be unilateral or bilateral.
Because of the rules of combination for root terms, the commonly used hyphenated [salpingo-oophorectomy] form of this word is not correct and should not be used.
Image modified from the original from Testut and Latajet, 1931. Public domain.
- Details
The term [scalpel] arises from the Latin word [scalpellum], meaning “a small knife”. Celsus (c.25BC - c.50BC) in De Re Medicina, uses the term [scalpellus] to refer to a surgeon’s knike.
The use of knives in Medicine is very old. 10,000 year old Mesolithic skulls have been found with craniotomies made with flint stone knives. The first one to describe surgical knives in recorded history was Hippocrates of Cos (460 BC - 370 BC).
Surgical knives were developed in a multitude of shape and forms, some of them veritable works of art. These scalpels were made by cutlery makers on demand by surgeons and had a fixed blade that had to be sharpened constantly, as surgery requires a very sharp blade.
The invention of the disposable razor by King Gillette in 1904 changed this. In 1910, Dr. John Benjamin Murphy (1857 – 1916) invented a handle that could hold a single-sided or a double-sided safety razor blade.
The design was improved by the invention of a disposable, sterilized surgical blade that could be easily installed on a reusable, sterilizable metal handle. Today sterile, disposable handle-blade combination scalpels of varying shapes and sizes are available, ensuring the surgeon the sharpest scalpel every time.
Sources
1. “The surgical knife” Ochsner J. Tex Heart Inst J. 2009; 36(5): 441–443
2. "History of the Surgical Blade" Shuja, A. Indep Rev Oct-Dec 2012;14(10-12)
3. "Masters of the Scalpel: The History of Surgery"" Riedman SR, R MacNally 1962
Images in the public domain, courtesy of Wikipedia
- Details
The [ureters] are two long, thin, bilateral muscular tubes that extend from the pelvis of the ipsilateral kidney to the posteroinferior aspect of the urinary bladder. The ureters are retroperitoneal structures and their function is the transport of urine between the kidney and the urinary bladder.
The word arises from the Greek [ουρητήρ], meaning "urinary duct". The term was originally used to denote both the urethra (in its singular form) and the ureters (in its plural form). Because of the problems using the term, the word [urethra] was created.
The ureter is composed of three layers: a mucosa, a thick muscular layer, and an adventitia. The muscular layer is itself composed of an deep longitudinal layer and a superficial circular layer formed by spiral smooth muscle fibers. In the distal portion of the ureter there is a third layer added to the ones mentioned, a thick longitudinal layer that extends into the walls of the urinary bladder. Since the ureter is a retroperitoneal organ, in the areas where the ureter is in contact with the parietal peritoneum, it can be said that the ureter presents with a fourth layer. The muscular construction of the ureters in layers allows for peristalsis that helps the flow of urine.
In the female the pelvic ureter passes just inferior to the uterine artery, as situation that surgeons refer to as "water under the bridge". Proper identification of the ureter is critical to avoid damage to this structure during a total hysterectomy. Surgeons will use the peristaltic movement of the ureter to identify it.
In its trajectory the ureters descend anterior to the psoas major muscle, pass over the pelvic brim, just anterior to the origin of the internal iliac artery, then hug the lateral pelvic wall and enter the urinary bladder from a posteroinferior aspect. As it descends the ureters receive blood supply from different arteries: renal arteries, gonadal (testicular or ovarian) arteries, aorta, common iliac arteries, and the inferior vesical arteries.
The ureters receive sympathetic and parasympathetic innervation from the autonomic nervous system renal plexus. Pieretti (2018) described the presence of intramural neuronal bodies (ganglionated plexi) within the ureter.
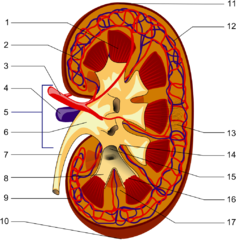
The image shows the longitudinal section of a kidney. 1-Renal pyramid, 3-Renal artery, 4-Renal vein, 5-Renal hilum, 6-Renal pelvis, 7- Ureter, 8-Minor calyx, 9-Renal capsule, 14-Minor calyx, 15- Major calyx, 16-Renal papilla, 17-Renal column .
Sources
1. "Gray's Anatomy"38th British Ed. Churchill Livingstone 1995
2. "Tratado de Anatomia Humana" Testut et Latarjet 8 Ed. 1931 Salvat Editores, Spain
3. "The origin of Medical Terms" Skinner, AH, 1970
4. "Histology; a Text and Atlas" Ross MH 3rd Ed. Williams and Wilkins 1995
Images in the public domain, courtesy of Wikipedia
- Details
The root term [-mamm-] arises from the Latin [mamma] (Pl. mammae), meaning "breast". The synonymous term [-mast-] arises from the Greek. This prefix is used in medical terms such as:
- Mammal: An animal with breasts or that feeds trough breast milk
- Mammary: Pertaining to the breast
- Mammoplasty: The suffix [-(o)plasty] is used to mean "surgical reshaping". Surgical reshaping of the breast. Can also be referred to as a mastoplasty
- Mammogram: The suffix [-(o)gram] means "to record", or "to write". The results of a breast examination, usually a film obtained with imaging technology
- Mammography: The suffix [-(o)graphy] means "to record", or "to examine". A breast examination, usually with imaging technology
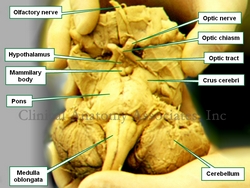
- Mammillary bodies: Two small, round structures found in the anterior aspect of the mesencephalon (midbrain) between the crura cerebri. See accompanying image. Click on the image for a larger depiction.
- Mammillary processes: Also known as the mammilary tubercles. These are small bony processes found in the transverse processes of the lumbar vertebrae
Image property of: CAA.Inc.Photography: E. Klein
- Details
This article is part of the series "A Moment in History" where we honor those who have contributed to the growth of medical knowledge in the areas of anatomy, medicine, surgery, and medical research.
William T.G. Morton
William Thomas Green Morton (1819-1868). American dentist, was born in Charlton, MA. In 1840, He started his studies at the Baltimore College of Dental Surgery. Interestingly, he left college without graduating to study with Horace Wells, DDS, in Hartford, CT. He started Medical school at Harvard, and left without graduating. In 1852 Morton received his honorary MD degree.
In 1846, Morton was able to successfully and painlessly extract a tooth from a patient under ether administration. To this effect he used an ether inhaler of his own invention that he called “Letheon”. This led to his now-famous demonstration of the use of ether as an anesthetic on October 16,1846 at the Massachusetts General Hospital first operating room, today known as the "Ether Dome". This is the first-ever recorded use of anesthesia as a way to reduce or eliminate pain in surgery, one of the revolutions in surgery, the other being Lister’s antiseptic technique.
Morton tried, unsuccessfully, to establish a patent on his discovery against Horace Wells (1815 – 1848). The litigation costs led him to poverty and he died with no money on 1868.
Although the American Dental Association in 1864 passed a formal resolution stating that Horace Wells was the discoverer of anesthesia, the name of William TG Morton has been tied to it since.
Sources
1. “William Thomas Green Morton (1819-1868” Keys. TE. Anesth and Analg (1973) 52: (2) 166
2. ” Morton, dentist, who first publicly demonstrated ether anesthesia; a short biography” Archer WH, William TG. J Am Dent Assoc. 1946 Dec 1;33(23):1528-32
3. “Horace Wells: Discoverer of Anesthesia” Jacobsohn PH. Anesth Prog (1995) 42:73-75
4. “The last days of William Thomas Green Morton” Vandam LD J Clin Anesth (1996) Sep;8(6):431-4334
- Details
A [lung] is one of the two main respiratory organs. It is an organ filled with minute air sacs or alveoli, giving its parenchyma the look and feel of a spongy tissue. Its function is the reoxygenation of blood.
Each lung is located on each side of the thoracic cavity, each one surrounded by a serosa membrane called "pleura". The pleura forms a sac that surrounds the lung and also lines the thoracic wall. The pleura that lines the thoracic wall is called "parietal pleura", while the pleura that lines the lung is called the "visceral pleura". An extension of the visceral pleura inferior to the pulmonary hilum forms the pulmonary ligament.
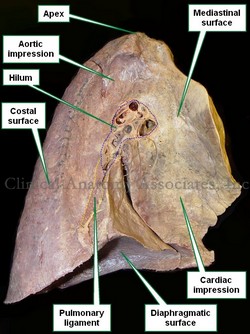
A lung has three surfaces and an apex. The inferior surface, base, or diaphragmatic surface; the medial surface or mediastinal surface, as if forms the lateral wall of the mediastinum; and the lateral or costal surface.
The lungs are also divided into lobes. The right lung has three lobes: superior, middle, and inferior while the left lung only has two lobes: superior and inferior. Because the heart has a left-sided tilt the left lung is slightly smaller than the right lung.
There are four structures that enter or leave the lung and they are found at the pulmonary hilum in the medial surface of the lung. These structures are: the main or primary bronchus, the pulmonary artery, and two pulmonary veins.
After entering the lung through the hilum each bronchus will divide into smaller and smaller bronchi eventually opening into microscopic air sacs called the alveoli. Each alveolus or alveolar sac is surrounded by capillaries. It is here where gas exchange takes place allowing for blood reoxygenation.
When examined, a lung will show the impressions of the organs that are in contact with it. Click on the accompanying image and you will be able to see the impressions left by the aorta and the heart
Image property of: Photographer: David M. Klein